Are you experiencing pain in your shoulder? Perhaps, your movement in that shoulder is also limited. If this is the case, you may be suffering from frozen shoulder, also known as adhesive capsulitis.
Cleveland Clinic explains the condition got the name frozen shoulder “because the more pain that is felt, the less likely the shoulder will be used.” By not using the shoulder, it will become tight and ultimately make the shoulder even more difficult to move, notes the source. Luckily there are ways to treat it. But there’s a lot more to know about this painful condition. Let’s take a look at the common signs and symptoms, causes, and treatment options for adhesive capsulitis.
What Is Adhesive Capsulitis (Frozen Shoulder)?
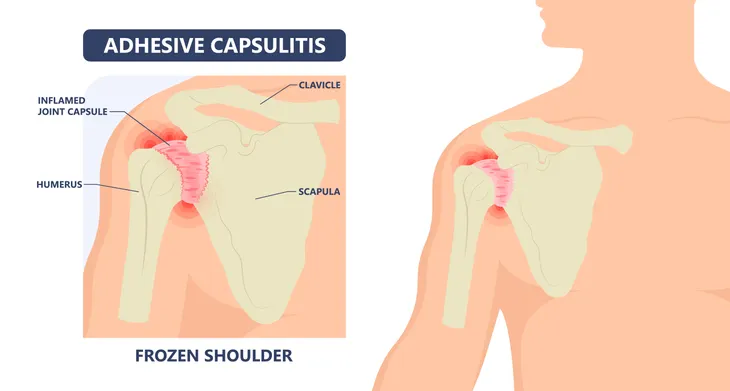
Adhesive capsulitis is a painful condition that affects your shoulder joint. The shoulder is a complex area made up of three bones (humerus, scapula, and clavicle) that form a ball and socket joint. Tissue surrounds the joint to keep everything in place and this is called the shoulder capsule.
Healthline explains, when adhesive capsulitis develops, “the tissues in your shoulder joint become thicker and tighter, scar tissue develops over time.” The scar tissue can make it difficult to rotate the shoulder properly ultimately leading to loss of range of motion.
Signs and Symptoms of Adhesive Capsulitis
The telltale sign of adhesive capsulitis is a pain in the shoulder. As the condition progresses, the pain will cause you to restrict your movements. By not moving your shoulder, it’ll start to get stiff and eventually lead to a loss of range of motion.
Once it progresses, reaching for items may become difficult. In severe cases, it can even interfere with your daily activities such as getting dressed. You typically go through three phases which we’ll look at next.
The Three Stages of Adhesive Capsulitis
The first stage is called the “freezing” stage in which you’ll develop pain in the shoulder. The pain is especially felt when you move the shoulder. Over time, it will slowly get worse and you may begin to be limited in how far you can move the shoulder. Some individuals also report the pain is more severe at night. This stage can last anywhere from 6 to 9-months.
The “frozen” stage is the second stage. While the pain may begin to subside, the stiffness often gets worse making daily activities more difficult. This stage can last anywhere from 4 to 12-months.
The final stage is known as the “thawing” stage and this is when your range of motion begins to get better. For some, this stage can last 6-months while it may take up to 2-years for others. The good news is your shoulder should fully or almost fully recover to its normal range of motion and strength.
What Causes Adhesive Capsulitis?
Adhesive capsulitis develops when “the tissue in your shoulder joint tightens and restricts movement,” says the Family Doctor. But what causes the tightness in the first place is most often an injury such as a rotator cuff injury or a broken arm.
Recovering from surgery or using your shoulder the wrong way can also cause adhesive capsulitis to develop. Certain factors can also increase your risk for developing the condition so let’s take a look at these next.
Risk Factors
First, frozen shoulder is more likely to occur in middle-aged individuals (around 40-years and older). It’s also more common in women.
If you have a thyroid disorder, are experiencing hormonal changes, or if you have diabetes, you have an increased risk of developing it. In fact, the Cleveland Clinic says, “between 0 and 20 percent of individuals with diabetes mellitus develop frozen shoulder.”
Other health conditions can also increase your risk. Parkinson’s disease, heart disease, a stroke, or a shoulder injury can all play a role in the development of adhesive capsulitis.
When to See a Doctor
If you ever develop persistent pain and stiffness in your shoulder you should book an appointment with your doctor. Your doctor will be able to assess the situation and your range of motion through a physical exam.
Your doctor may ask you to perform certain movements (such as touching your opposite shoulder with your hand) in order to measure your range of motion. They may also ask you about your medical history and order a variety of tests to diagnose adhesive capsulitis.
Diagnosis
To diagnose frozen shoulder, your doctor will likely start with a physical exam to review your symptoms and your current range of motion. If a physical exam isn’t sufficient enough for a diagnosis, your doctor may also need to perform a few tests.
For starters, a magnetic resonance imagining (MRI) scan may be necessary to rule out a rotator cuff tear. X-rays or an ultrasound may also be required to check for any abnormalities as well as arthritis. Healthline notes, “you may need an arthrogram for the X-ray, which involves injecting dye into your shoulder joint so that the doctor can see its structure.”
Treatment
Healthline says, although you can leave frozen shoulder untreated, the pain and stiffness can last for several years. So it’s better to deal with it head-on.
Once you’ve been diagnosed with frozen shoulder, your doctor can recommend a treatment plan which may include physical therapy, medication, or surgery. Your doctor may also provide a list of at-home treatments. Let’s take a closer look at these options next.
Physical Therapy
The most common form of treatment for adhesive capsulitis is physical therapy. Physical therapy can help you regain motion in your shoulder, although treatment can take several weeks or months to see progress.
Along with your appointments, your physiotherapist will likely provide you with a list of exercises you can do safely at home to further your treatment. Healthline says, if you don’t see progress after 6-months, you should talk to your doctor about other treatment options.
At-Home Treatments
While you follow the guidance of your doctor there are some at-home treatments you can start doing to help. For starters, you may find relief from the pain by placing an ice pack on your shoulder for 15-minute increments a few times per day. Over-the-counter pain relievers may help with the pain as well.
The American Association of Orthopaedic Surgeons says simple and gentle at-home exercises can also help. One exercise you can try is the crossover arm stretch. This involves holding the upper arm of the affected side and then gently pulling the arm across in front of you, under the chin. Hold that position for 30-seconds and then relax before repeating. Keep in mind, the exercises you perform should be guided by your doctor or physical therapist.
Surgery
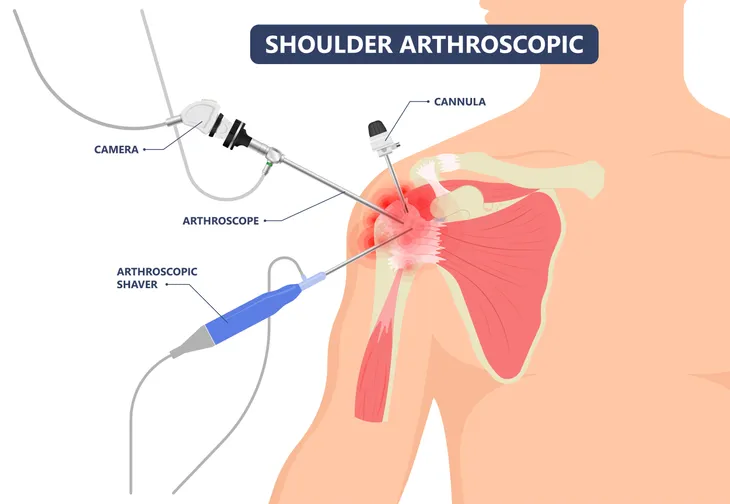
If at-home treatments and physical therapy fail to help your condition, then surgery may be necessary. The American Association of Orthopaedic Surgeons says surgery is usually an option during stage two, “frozen.” The ultimate goal of surgery is “to stretch and release the stiffened joint capsule,” says the source. And the most common methods are shoulder arthroscopy and manipulation under anesthesia.
During shoulder arthroscopy, the surgeon will cut through tight sections of the joint capsule using small instruments that are inserted through a small incision on your shoulder. In contrast, manipulation under anesthesia is a procedure where you’ll be put to sleep. During this procedure, the surgeon will force your shoulder to move, causing the capsule and scar tissue to either stretch or tear. This will decrease the tightness and increase your range of motion.
The source also notes that both procedures are often used in combination in order to achieve maximum results.
What Is the Outlook?
The good news is the overall outlook of adhesive capsulitis (frozen shoulder) is good. Healthline says many individuals recover within 2-years without treatment but at-home treatments, physical therapy, and pain medications can all help speed up the process.
If surgery is necessary, be sure to follow the guidance of your doctor, especially post-op. It’s important that you continue doing your therapy exercises to ensure the condition doesn’t return.