Any way you look at them, problems with the bowel are not pleasant. However, while there are common health problems associated with the bowel that sound somewhat similar, there are some key differences.
In particular, we’re talking about irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD), which share some features but have different causes and symptoms. Let’s take a closer look at the 13 key differences between the two…
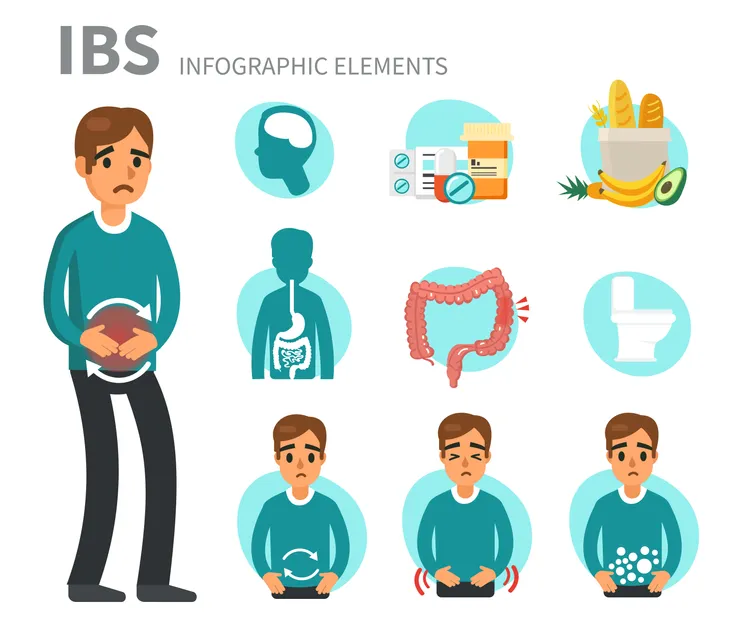
Defining IBS
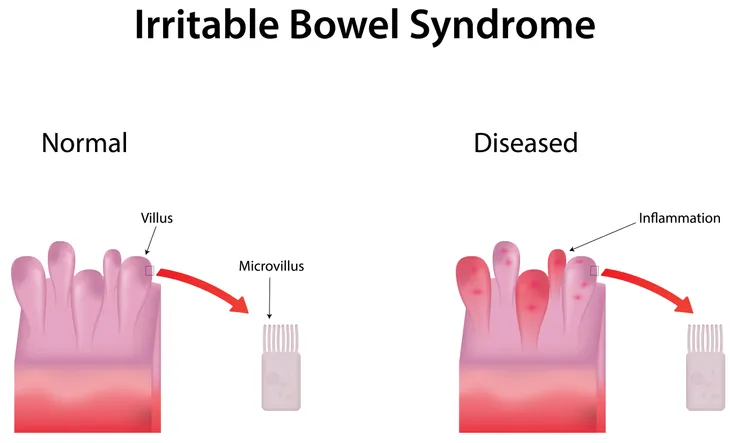
This is something doctors refer to as a “functional disease,” which means if a doctor looks at scans of your gut, they probably won’t be able to tell there’s anything wrong physically notes WebMD.
Instead, the patient will report a group of symptoms, which makes it a syndrome and not a disease – “tests won’t show any physical explanation for those problems,” says the source.
Defining IBD
WebMD says IBD is a “structural disease,” meaning there’s some kind of physical damage that’s causing the problem. If a doctor performs a scan or endoscopy of your bowel, they will see chronic inflammation or ulcers (sores) if you have IBD.
The source notes that both Crohn’s disease and ulcerative colitis are considered examples of IBD, both with their own unique characteristics and challenges.
Some Shared Symptoms
Both of these conditions can be hard to distinguish, as they can have similar symptoms, according to Healthline.com. For example, both IBS and IBD can cause abdominal pain and cramping, constipation, or diarrhea. They can both also cause “urgent bowel movements,” adds the source.
You may also find you have excessive gas with either condition. However, IBD can present a host of other symptoms that you may not associate with the bowels, notes Healthline, which we’ll take a closer look at next.
Unique Symptoms of IBD
Healthline also notes that there are a number of symptoms of IBS that won’t be present if you have IBD. For example, the source says you can get seemingly unrelated problems such as eye inflammation and joint pain if you have IBD.
IBD can also cause unique problems, such as extreme fatigue, malnutrition, weight loss, rectal bleeding, and intestinal scarring. Other health issues can cause these symptoms as well, so it may be best to let a doctor sort it out.
The Subtypes of IBD
IBD is an umbrella term for a range of diseases that affect the gut. As we mentioned before, the two main categories of IBD are ulcerative colitis and Crohn’s disease.
The Mayo Clinic explains ulcerative colitis leads to “long-lasting” inflammation and sores (ulcers) in the innermost lining of your colon and rectum. Crohn’s disease is inflammation of the digestive tract, “which often spreads deep into affected tissues,” the source adds.
How IBS is Diagnosed
Since IBS doesn’t have the obvious physical markers that IBD does, it takes a slightly different approach to diagnosis, according to WebMD. The source says the “Rome criteria” are applied to arrive at a diagnosis of IBS.
This criteria dictates you have IBS if you’ve experienced abdominal pain for at least 1-day per week over the previous 3-months. Changes in bowel movement frequency when the pain begins, or a physical change in your stool when experiencing pain, are both also markers for a diagnosis, adds the source.
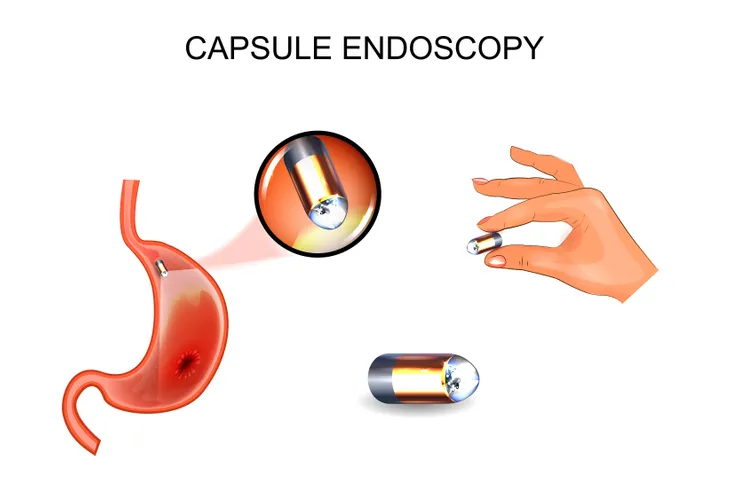
How IBD is Diagnosed
The Crohn’s & Colitis Foundation of America explains the gold standard for the diagnosis of IBD is endoscopy and biopsy. The endoscope is equipped with a tiny camera that lets doctors have a better look inside your intestines to see if inflammation is present.
“Although laboratory tests support the diagnosis of IBD, endoscopy plays the most important role,” it explains. That being said, doctors often use blood tests as part of the process. While blood tests won’t pinpoint IBD directly, they can show evidence of inflammation in the body. Stool tests can also be used to rule out other health problems.
The Underlying Causes of IBS
The Mayo Clinic says the exact cause of IBS isn’t clear, but the medical community believes there are some contributing factors. They include muscle contractions in the intestine during digestion that are stronger or weaker than normal, as well as “abnormalities” in the nerves of the digestive system.
The source also notes some patients with IBS have more immune cells than normal in their intestines, and an immune response may be responsible for pain and diarrhea. Other theories include that IBS can occur after a severe bout of diarrhea, or it could be associated with a “surplus of bacteria in the intestines.” IBS might also indicate that the “good bacteria” in the gut (microflora) are out of balance.
Possible Causes of IBD
In the case of IBD, it could be related to an autoimmune response, says WebMD. While it has been thought the chronic inflammation of IBD was a result of the immune system attacking the body itself, research suggests it is a “result of the immune system attacking a harmless virus, bacteria, or food in the gut, causing inflammation that leads to bowel injury,” adds the source.
The source says recent studies have pointed to “some combination of hereditary, genetic, and/or environmental factors” leading to the development of IBD. In any case, it’s not exactly known what causes the disease.
How Common are IBS and IBD?
When it comes to prevalence, IBS is “extremely common,” notes Healthline. How common? The International Foundation for Functional Gastrointestinal Disorders estimates it affects up to 15-percent of the population worldwide – and about 25-percent of Americans report IBS symptoms.
While the literature doesn’t give a solid number for IBD, it notes a person diagnosed with IBD can complain of IBS-like symptoms. “It’s also important to know that you can have both conditions at the same time,” adds Healthline.
The Stress Connection
Healthline says that stress may be a contributing factor to both IBS and IBD, while “IBS is almost always exacerbated by stress.” It adds that IBD may flare up in low-stress or high-stress situations.
The source suggests natural stress reduction techniques that include meditation, regular exercise, talk therapy, and yoga to help keep the symptoms to a minimum.
Colon Cancer Risk
The Crohn’s & Colitis Foundation notes there could be a greater risk of colorectal cancer tied to patients with IBD (both Crohn’s disease and ulcerative colitis). The risk of colon cancer begins to increase once you’ve had IBD for 8 to 10-years. A family history of colorectal cancer can also play a role in increasing risks.
“Inflammation of the colon can cause continuous turnover of cells in the intestinal lining, increasing the risk of irregularities that may lead to colon cancer,” it explains. The good news is that colorectal cancer is “highly treatable when found early,” adds the source.
Treatment for IBS
Healthline explains IBS may be treated with certain drugs, including intestinal antispasmodics such as hyoscyamine (Levsin) or dicyclomine (Bentyl). There are also natural remedies recommended for IBS, such as increasing the fiber in your diet, avoiding alcohol and spicy foods, and exercising regularly.
Meanwhile, treatment for IBD is dependent on what type it is, but the main goal is limiting inflammation that can damage the intestines. The source adds DIY remedies for IBD include avoiding dairy, alcohol, and spicy foods, while limiting your fiber intake.