The month of October is Spina Bifida Awareness Month.
The goal of the Spina Bifida Association is to increase the overall awareness of Spina Bifida as far as needs, research, and support in the community using the hashtag #BeyondAllLimits.
What is Spina Bifida
The latin translation for Spina Bifida is “split spine, it describes the most common birth defect in the United States—affecting roughly eight babies born daily.
According to the Spina Bifida Association (SBA), the permanently disabling brain and spinal birth defect, which occurs in the womb when the backbone and membranes around the spinal cord don’t close completely.
Neural Tube Defects
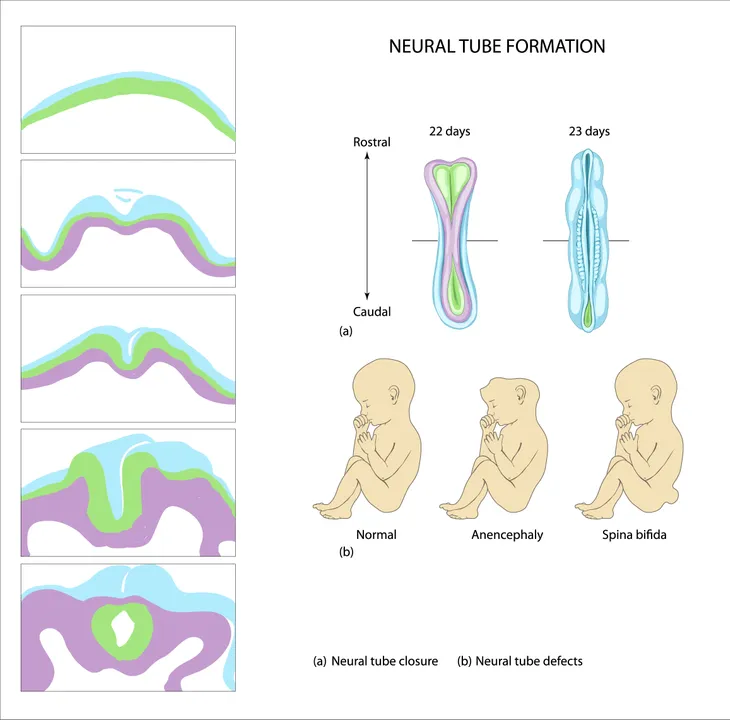
Spina bifida is classified by the Mayo Clinic as a type of neural tube defect. The neural tube, or embryonic structure, forms during early pregnancy and closes typically 28 days after conception.
However, in babies with spina bifida (and other neural tube defects) this embryonic structure that eventually encloses the fetus’ brain and spinal cord develops improperly, leaving defects in the spinal cord and tissues and bones of the spine.
What Causes Spina Bifida?
Although scientists speculate a that environmental and genetic factors may play collaborative roles in spina bifida development, they cannot pinpoint a clear cause for the defect.
However, the Mayo Clinic explains that spina bifida may be linked to a combination of family history of (genetic) neural tube defects and folic acid deficiency (environmental) factors.
Forms and Severity
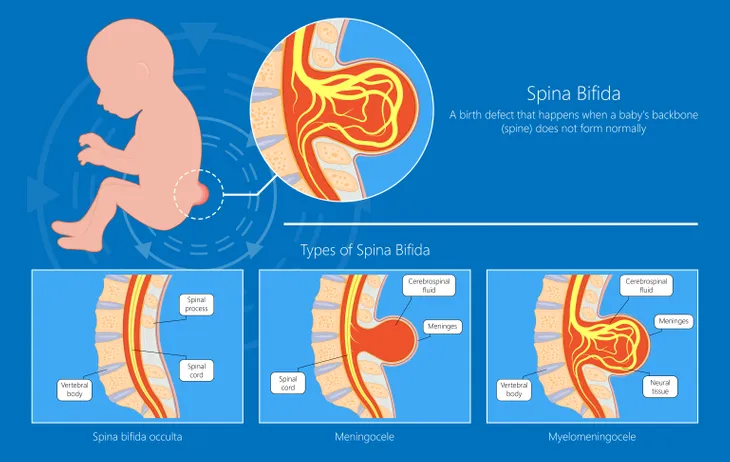
Spina bifida cases vary in severity and form. For instance, the Spina Bifida Association identifies four different types of spina bifida—Spina Bifida Occulta (or hidden spina bifida), which is the mildest form and only causes small gaps in the spinal vertebrae and causes few visible symptoms; Occult Spinal Dysraphism (or OSD), which develops as a small dimple on a baby’s lower back and can cause redness, tufts of hair, small lumps, or hyper-pigmented patches due to the improper growth of the spinal cord.
Meningocele is a form of spina bifida that causes minor disability due to the emersion of the spinal cord and nerve fluid sac through the spine; and Myelomeningocele (or Spina Bifida Cystica), the most severe form, which occurs when the spinal cord and nerves emerge through an open gap in the spine and results in nerve damage, fluid on the brain, and potential brain damage.
Spina Bifida Risk Factors
Although a clear cause of spina bifida is unknown, Mayo Clinic researchers note a prevalence for the birth defect among certain races (i.e., Hispanic), genders (i.e., female), and among families with a history of neural tube defects.
In addition, the Mayo Clinic notes that certain environmental factors—such as women with diabetes, taking anti-seizure drugs (i.e., Depakene), folate deficiency, pre-pregnancy obesity, and higher than normal body temperature (or hyperthermia) during early pregnancy—may increase the risk of spina bifida.
Spina Bifida Testing and Treatment
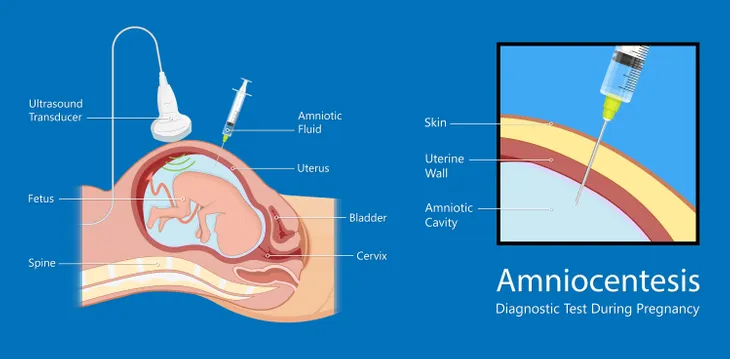
There are three tests that can detect spina bifida in babies prior to birth. First, a maternal amniocentesis uses a thin needle to extract fluid from the womb to test for protein levels. Secondly, an ultrasound can detect the presence of an open spine. Thirdly, an alpha-fetoprotein blood test can screen for spina bifida between week 16 and 18 of pregnancy.
Surgery is an option for babies born with Meningomyelocele spina bifida during the first few days after birth to prevent further spinal cord damage, as well as infections. Children born with Occult Spinal Dysraphism (or OSD) may require surgery to prevent further brain and nerve damage as they grow.
Spina Bifida Prognosis
The Spina Bifida Association notes that between 90- and 75-percent of children born with the birth defect attend school, are physically active, and thrive into adulthood.
Depending on the severity, ongoing treatments and surgeries may be required by a collaborative team of psychologists, occupational therapists, physical therapists, urologists, neurosurgeons, and orthopedists.