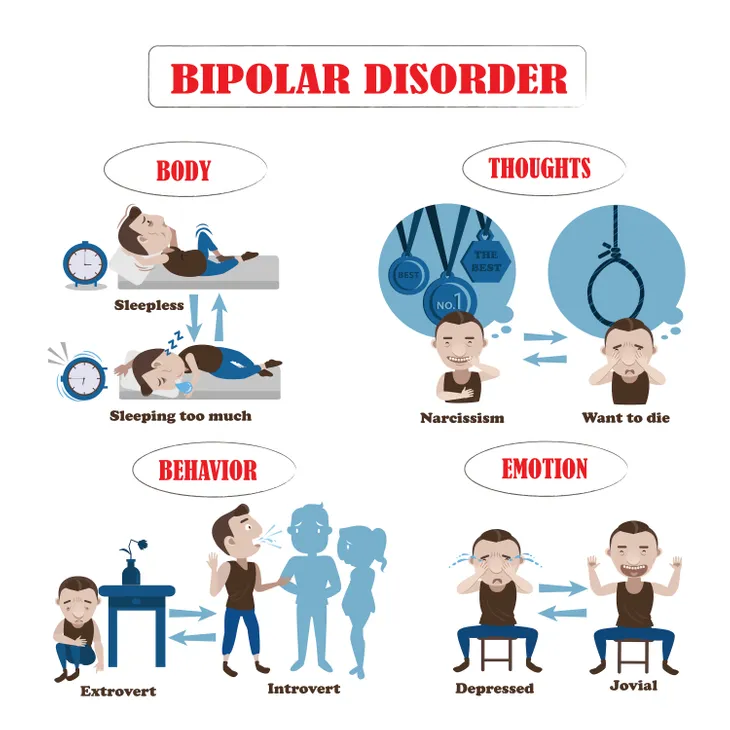
Bipolar disorder is a mental disorder that consists of manic and depressive episodes which are essentially periods of high and low moods. While the symptoms tend to vary from person to person, overall these episodes are known to be accompanied by other symptoms that affect their energy levels, mood, activity levels and the ability to carry out day-to-day tasks.
Bipolar disorder is a very complex condition that can be difficult to deal with. Similar to many other illnesses, it not only affects the person who’s been diagnosed, but also anyone close to them like friends and family. A diagnosis isn’t always easy and that’s because there are seven different classifications of bipolar disorder: bipolar I disorder (manic-depressive disorder), bipolar 2 disorder (hypomania), cyclothymia, rapid cycling, and substance/medication-induced bipolar and related disorder, bipolar and related disorder due to another medication condition, other specified bipolar and related disorder, and unspecified bipolar and related disorder.
To simplify things, we’ve compiled a list of everything there is to know about bipolar disorder and each of the different classifications. Let’s take a look…
What is Bipolar I Disorder?
Bipolar I disorder is also sometimes referred to as manic-depressive disorder or manic depression. It’s a form of mental illness that refers to a person who suffers from, or has experienced at least one manic episode in his or her life. WebMD defines a manic episode as “a period of abnormally elevated mood and high energy, accompanied by abnormal behavior that disrupts life.”
People who suffer from bipolar I disorder often also suffer from depression or episodes of depression. These episodes of mania and depression can occur back and forth creating a cycling pattern which is why the term “manic depression” was coined. While this condition might sound like it is debilitating (and it’s definitely not easy), people who have this condition can live relatively normal lives in between their manic and depressive episodes.
Symptoms of Bipolar I Disorder
Now that we’ve discussed what bipolar I disorder is, how do we recognize it? A manic episode is an “elevated mood [that] can manifest itself as either euphoria (feeling ‘high’) or as irritability,” writes WebMD. This euphoric mood is accompanied by behavioral signs like jumping from one idea to the next, increased energy, lack of sleep, rapid and loud speech, inflated self-image, reckless behavior like excessive spending, drinking, substance abuse, or even hyper-sexuality.
On the opposite end of the spectrum, there are depressive episodes that look very similar to clinical depression. This includes low energy and activity, sadness, feelings of guilt and worthlessness, and thoughts of suicide.
In both of these cases the symptoms can last for a few weeks or months. When a bipolar patient experiences a manic episode it might mean that a depressive episode will follow soon after, but there can be long periods between these episodes where the patient exhibits no symptoms at all.
Who’s at Risk for Bipolar I Disorder?
WebMD estimates about 2.5-percent of the U.S. population suffer from bipolar disorder which is about six million people. That’s a lot of people! What’s even scarier is that bipolar I disorder could happen to virtually anyone. There aren’t many risk factors that pinpoint whether someone will be diagnosed or is at risk. The main risk factor is family history. If an immediate family member has been diagnosed, then their close relatives are at a higher risk.
While this doesn’t narrow it down much, in addition to family history, age can play somewhat of a factor. Almost every person who’s developed bipolar I disorder has done so before the age of 50. Symptoms typically begin to appear in the teenage years or early twenties.
Treatment for Bipolar I Disorder
For the most part, bipolar I disorder is treated with medication. Manic episodes are often treated with mood stabilizers, antipsychotics, and sometimes sedative-hypnotics, whereas depressive episodes are treated with antidepressants. WebMD also notes that “people with bipolar I disorder (mania or depression) have a high risk for recurrences and usually are advised to take medicines on a continuous basis for prevention.”
Lastly, there is electroconvulsive therapy (ECT). While this method tends to have a bad reputation, according to WebMD, it’s actually a safe and effective treatment. “ECT is often used to treat severe forms of depression or mania in bipolar I disorder when medicines may not be effective or likely to work fast enough to bring symptom relief.”
What is Bipolar II Disorder?
Bipolar II disorder is closely linked to bipolar I disorder because they share a similar cycle of high and low moods. The biggest distinction between the two revolves around the elevated moods which for bipolar II disorder patients, are not nearly as severe. WebMD explains that in “bipolar II disorder, the ‘up’ moods never reach full-blown mania. The less-intense elevated moods in bipolar II disorder are called hypomanic episodes, or hypomania.”
A person can be diagnosed with bipolar II disorder if the patient has experienced at least one hypomanic episode in his/her life. Similar to bipolar I disorder, the hypomanic episodes are often followed by an episode of depression which is why it’s referred to as “manic depression.” In between all the highs and lows, someone who suffers from bipolar II disorder is able to live a relatively normal life.
Symptoms of Bipolar II Disorder
As previously mentioned, the two most common indicators of bipolar II disorder are the high and low moods which are categorized as hypomanic and depressive episodes. These episodes are accompanied by their own symptoms. For example a hypomanic episode is an “elevated mood [that] can manifest itself as either euphoria (feeling ‘high’) or as irritability.”
This incredibly happy mood will include rapid speech, a jumpy mentality that bounces from idea to idea, an exaggerated sense of self confidence, and an increased energy with a decreased need for sleep. “Hypomanic episodes can sometimes progress onward to full manias that affect a person’s ability to function (bipolar I disorder). In hypomanic episodes, people might spend money they don’t have, seek out sex with people they normally wouldn’t, and engage in other impulsive or risky behaviors with the potential for dangerous consequences,” writes WebMD.
What’s unique about bipolar II is that patients who suffer from this type of bipolar disorder will experience more or longer depressive episodes than they will hypomania. Depression can occur immediately after a hypomanic episode, but not always, and there can be long lapses of time in between and it varies from person-to-person. These depressive episodes look a lot like clinical depression with low energy, activity, feelings of guilt and worthlessness, as well as a loss of pleasure and overall sadness. Both episodes have the ability to last for either weeks or months, but rarely years. And again, the time in between can vary greatly.
Who’s at Risk for Bipolar II Disorder?
The risk factors for bipolar II disorder are the exact same as bipolar I disorder. The only two known factors to pay attention to are family history and age. Many of the symptoms begin to appear when the patient is in their teenage years or early twenties and it’s extremely rare for the disorder to develop after the age of 50.
In addition to this, if someone in your immediate family suffers from bipolar disorder, you are at a higher risk than someone who does not have a family history of this mental illness.
Treatment for Bipolar II Disorder
One of the hardest things about diagnosing and treating bipolar II disorder is that hypomania appears as happiness and joy, so it often goes unnoticed. But there’s a lot more to hypomania than these happy-go-lucky feelings, and some of the effects can actually be quite negative which is why it needs to be treated, especially before it turns into full blown mania which typically requires medication, and sometimes even hospitalization.
WebMD notes that bipolar II disorder can sometimes be treated with preventative drugs that level out moods over time. These drugs will help protect against the negative effects of hypomania and from the depression that follows.
What is Rapid Cycling Bipolar Disorder?
Rapid cycling refers to a pattern of distinct episodes within the disorder and not necessarily the symptoms associated with these episodes. A bipolar patient is diagnosed with bipolar disorder with rapid cycling if they’re experiencing four or more mood swings within about 12-months. “In rapid cycling, a person with the disorder experiences four or more episodes of mania or depression in one year. It can occur at any point in the course of bipolar disorder, and can come and go over many years depending on how well the illness is treated; it is not necessarily a ‘permanent’ or indefinite pattern of episodes,” writes WebMD.
VeryWell Mind explains that these episodes consist of depression, mania, hypomania, or what’s called a ‘mixed state’ where mania and depression occur at the same time. Most people who suffer from rapid cycling bipolar disorder alternate between manic and depressive episodes about twice a year while others only have these episodes once every few years. There’s also a small group of people who experience them more frequently and the episodes come on much quicker.
Symptoms of Bipolar Disorder with Rapid Cycling
Bipolar disorder with rapid cycling is a form of bipolar disorder that consists of different patterns of distinct episodes. These mood swings can be unpredictable and random, and there’s usually no rhyme or pattern behind them. They could occur quite frequently on a weekly or monthly basis, or only every few months. It is different for each person.
The rapid cycling episodes aren’t much different than any other form of bipolar disorder. In fact, the only real difference is the speed at which these episodes occur. VeryWell Mind notes that researchers are still unsure why rapid cycling disorder occurs, nor can they predict how long it will last, or if there is any clear pattern between these episodes. “While some rapid cyclers will often alternate between depression and hypomania (a less severe form of mania), most cases will be dominated by episodes of depression,” says the source. It can sometimes be difficult to recognize because some patients have episodes that are mixed or in a mild hypomania state, which means they are shorter and less severe.
Who’s at Risk for Bipolar Disorder with Rapid Cycling?
Similar to the other types of bipolar disorder, pretty much anyone can develop bipolar disorder with rapid cycling, but it’s more likely to occur in someone who has a family history of mental illness, particularly with bipolar disorder. It begins to develop in teenage years and early twenties and is rarely diagnosed past the age of 50.
According to WebMD, about 2.5-percent of the U.S. popular suffer from some form of bipolar disorder and rapid cycling accounts for about 10 to 20-percent of bipolar cases. The same source says it’s more common among women and people who’ve been previously diagnosed with bipolar II disorder.
Treatment for Bipolar Disorder with Rapid Cycling
Not surprisingly, bipolar disorder with rapid cycling is a lot harder to treat than others. Since depression seems to be the dominating episode within rapid cycling bipolar disorder, most of the treatment is focused on “stabilizing mood, mainly by relieving depression while preventing the comings-and-goings of new episodes,” writes WebMD.
For the most part antidepressants have been proven to be not as effective for patients with rapid cycling bipolar disorder. The more reliable option is mood stabilizers which are often used in combination with antipsychotics, says VeryWell Mind. Patients who have never been diagnosed with bipolar disorder might be put on lithium as a first-line of treatment, but mood stabilizers will be prescribed indefinitely as a way to prevent future episodes. If antidepressants are prescribed they will only be taken during a depressive episode and should be stopped as soon as it’s resolved.
What is Bipolar Disorder with Mixed Features?
Bipolar disorder with mixed features is exactly what it sounds like. The episodes that patients experience are a mix of depression and mania. For the most part, this is the main difference between this form of bipolar disorder and the others on this list.
All of the other forms of bipolar disorder experience both depression and mania (or a milder form of each), but none of them will have episodes that occur simultaneously. If not experienced at the same time, these mixed episodes can also occur on top of each other, meaning one right after another in a rapid sequence.
Symptoms of Bipolar Disorder with Mixed Features
Since we’ve already established that mixed features are when someone experiences highs and lows at the same time, now we ask…how is that possible? These two emotions are polar opposites, so how can they be experienced at the same time without any recovery in between? WebMD explains, “mania with mixed features usually involves irritability, high energy, racing thoughts and speech, and overactivity or agitation.” On the other hand, depression with mixed features has the same symptoms as regular depression which would include “feelings of sadness, loss of interest in activities, low energy, feelings of guilt and worthlessness, and thoughts of suicide.”
It seems like it’s impossible to be depressed and ecstatic at the same time, but the co-occurrence of these symptoms happens more than you’d think. For example a patient might be crying while saying they’ve never felt better in their entire life or be extremely happy, and then all of the sudden be extremely miserable, only to return to being happy a few minutes later. These confusing and exhausting episodes can last anywhere from a few days to a few weeks, or even months if left untreated. “They may recur and recovery can be slower than during episodes of ‘pure’ bipolar depression or ‘pure’ mania or hypomania.”
Who’s at Risk for Bipolar Disorder with Mixed Features?
Mixed features is a common occurrence with people who’ve been diagnosed with bipolar disorder. In fact, half or more of people with bipolar disorder will experience some kind of mixed features where they have mania symptoms during an episode of depression. Also, patients who develop bipolar disorder at a young age like in their adolescent years are more likely to experience mixed features. “People who develop episodes with mixed features may also develop ‘pure’ depressed or ‘pure’ manic or hypomanic phases of bipolar illness,” writes WebMD.
WebMD also points out that some people will experience a major depression won’t have full blown mania or hypomania but rather low-grade mania symptoms. “These are symptoms that are not severe or extensive enough to be classified as bipolar disorder. This is referred to as an episode of ‘mixed depression’ or a unipolar (major) depressive episode with mixed features.”
Treatment for Bipolar Disorder with Mixed Features
Bipolar disorder with mixed features can be a complicated thing to treat and often takes a bit of mixing and matching between mood stabilizers and atypical antipsychotics in order to find the right treatment. VeryWell Mind explains that antidepressants are usually always avoided because they tend to trigger acute manic episodes.
In a last case scenario, if medication seems to be ineffective, the same source notes that electroconvulsive therapy (ECT) can also be used to help provide relief from any episode with mixed features.
What is Cyclothymic Disorder?
Cyclothymia (sometimes referred to as cyclothymic disorder) is generally seen as a milder form of bipolar disorder. Even though it still consists of extreme mood swings and all the highs and lows of mania and depression with short periods of normalcy in between, the main difference is the level of intensity for each episode. Everyday Health explains that other forms of bipolar disorder will have episodes that are much more intense bouts of clinically diagnosed mania alongside major depression. Cyclothymia on the other hand is still a serious form of bipolar disorder, but it’s less noticeable and can sometimes just feel like a low-grade depression or mild hypomania.
“It may seem like you’re just going through a string of good days and a string of bad days,” says psychiatrist Kathleen Franco, MD, of the Cleveland Clinic Lerner College of Medicine in Cleveland while talking to Everyday Health. “But the mood shifts keep going, and there’s little neutral time in between.”
Symptoms of Cyclothymic Disorder
Since cyclothymia is a milder form of bipolar disorder, the symptoms aren’t quite as severe. The depression is much milder and the hypomania is less intense, but the pattern of episodes is still quite random and unpredictable. “Hypomania and depression can last for days or weeks. In between up and down moods, a person might have normal moods for more than a month — or may cycle continuously from hypomania to depression, with no normal period in between,” writes WebMD.
The source also notes that these depressive episodes never reach the levels of major depression and the hypomania never becomes full blown mania. As a result, it seems to be a fine line between cyclothymia being a mental illness as opposed to just normal variations in mood. “Some people with mild symptoms are highly successful in life, driven by their hypomania to express individual talents. On the other hand, chronic depression and irritability can ruin marriages and professional relationships,” says WebMD.
Who’s at Risk for Cyclothymic Disorder?
Cyclothymic disorder is quite rare. In fact, WebMD says that only 0.4 to 1-percent of the U.S. popular have been diagnosed with this form of bipolar disorder. It doesn’t seem to have any greater likelihood of developing in either men or women — both genders are equal in this case, but symptoms do tend to appear in the teenage years or early adulthood. Unfortunately, it’s also very hard to diagnose so it can go unnoticed and untreated for a long period of time.
Treatment Options for Cyclothymia
Unlike the other forms of bipolar disorder on this list, cyclothymia doesn’t need to be treated with antidepressants, mood stabilizers, or antipsychotics. In fact, they don’t usually work. A better form of treatment is talk therapy with a trusted psychologist “who can help people recognize the triggers that may increase the severity and frequency of their mood swings,” says Everyday Health. Cyclothymia is often triggered by things like lack of sleep, alcohol consumption, or even the jet lag that commonly accompanies travel. Cognitive behavioral therapy helps a patient identify what their triggers are and how to replace them with healthier behaviors.
If talk therapy doesn’t work or isn’t as effective as you’d like, the same source lists other options like interpersonal and social rhythm therapy which helps patients develop a stable daily routine of eating, sleeping, and exercise. There is also light therapy which is used to treat seasonal affective disorder. Because cyclothymia is linked to mood shifts, it could be helpful to regulate the body’s biological rhythms which is what light therapy aims to do. Lastly, anyone with cyclothymia or any other form of bipolar disorder should have some sort of support system, including their doctor.