Hormone replacement therapy (HRT) has been used to treat menopause symptoms for a long time now because it still to this day is the most effective treatment for menopausal symptoms like hot flashes and discomfort. The Mayo Clinic notes that HRT has also been found to prevent bone loss and reduce fracture.
However, since 2002 when the Women’s Health Initiative (WHI) trial discovered that hormone replacement therapy could increase a woman’s risk of breast cancer, heart disease, stroke, and blood clots, the number of women taking medication to treat their menopause dropped dramatically. Since then, the U.S. Food & Drug Administration and Health Canada require all estrogen prescriptions to carry a black-box warning of the risks.
The bottom line is that while there are benefits to hormone replacement therapy, there are also risks. There are many factors that need to be taken into consideration before a woman decides to use HRT to treat her menopause symptoms. Each woman is unique in not only her own symptoms, but also how she will respond to treatment. There are also a variety of factors that come into play when determining who is at risk. Some women are more eligible than others, and for some women, it’s safer. The only way to determine if it’s right for you, is to consult with a doctor.
Hormone Therapy Overview
Before we get into the details, we have to explain the two different types of HRT and two most common forms of treatment. The first type of HRT is estrogen-only therapy (ET). This form of treatment provides the best relief of menopausal symptoms, but it is only prescribed to women who do not have a uterus due to a hysterectomy, explains the North American Menopause Society (NAMS). The second type of HRT is EPT which is a combined treatment of estrogen and progestogen therapy. “Progestogen is added to ET to protect women with a uterus against uterine (endometrial) cancer from estrogen alone,” writes the source.
The two ways to take HRT are with systemic products that circulate through the bloodstream, like with a pill, patch, gel, cream or spray, and according to the Mayo Clinic, this “remains the most effective treatment for the relief of troublesome menopausal hot flashes and night sweats.” The second is local (nonsystemic) products that target a specific area of the body. The North American Menopause Society says this would come in the form of a cream, ring, or tablet and is more often used for vaginal symptoms.
Pros
Most Effective Treatment for Hot Flashes
So onto why HRT is prescribed to women in the first place. The reason is because it works — plain and simple. There have been hundreds of clinical studies over the years have found that “systemic HT (estrogen with or without progestogen) effectively helps such conditions as hot flashes, vaginal dryness, night sweats, and bone loss,” writes NAMS.
While there are obviously risks associated with hormone therapy, for some women, the benefits outweigh the risks. According to the Mayo Clinic, the criteria for being one of these benefiting women are someone who “experience moderate to severe hot flashes or other menopausal symptoms, have lost bone mass and either can’t tolerate or aren’t benefiting from other treatments, stopped having periods before age 40 (premature menopause) or lost normal function of your ovaries before age 40 (premature ovarian insufficiency).”
The source goes on to explains that women who enter early menopause, especially those who have had their ovaries removed and don’t take estrogen therapy before the age of 45 are at a higher risk for developing osteoporosis, heart disease, premature death, Parkinson’s-like symptoms, as well as anxiety or depression. “For women who reach menopause prematurely, the protective benefits of hormone therapy usually outweigh the risks,” writes the Mayo Clinic.
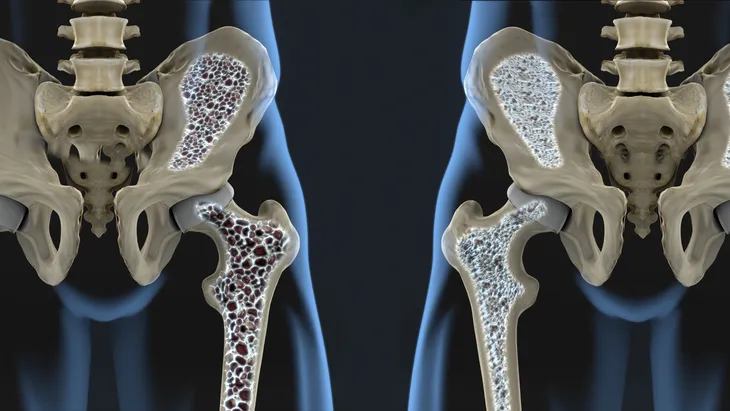
May Protect Against Osteoporosis
We’ve already mentioned that hormone therapy with estrogen and/or progesterone is often used to treat menopause, but it can also be used to treat osteoporosis. Osteoporosis Canada writes, “…because estrogen plays such an important role in maintaining bone, HT is another option to consider to treat osteoporosis if you are also seeking relief from symptoms of menopause.”
After menopause the body produces less estrogen and progesterone which reduces bone density. “Estrogen/progesterone treatment is not intended to ‘replace’ the loss of these hormones, but to supplement these hormones to the lowest level required to prevent bone loss.” This kind of treatment has been successful in preventing spine and hip fractures.
It Can Help with Dryness
Hot flashes are one of the most commonly known symptoms of menopause, but there are others! It can also cause unpleasant vaginal dryness which cause make sex and urination painful. A study conducted by the North American Menopause Society found that a third of women experience dryness, but only half of them tell their doctor and less than 4-percent receive treatment for it.
“Estrogen (generic estradiol or Vagifem) pills that are fired with a dispenser into the vagina, helps both dryness and urination problems,” writes Healthline. You can also use a ring device that releases estrogen in low doses over the course of three months, explains Robin Phillips, a New York gynecologist to the source. Dr. JoAnn Pinkerton, executive director of the North American Menopause Society and professor of gynecology at the University of Virginia Health System also chimes in on the subject by stating, “Estrogen in the vagina doesn’t pose any risk (or benefit) to the rest of the body, since it isn’t absorbed elsewhere. But you might hear otherwise from one of your doctors.” According to Pinkerton, some doctors don’t understand that “only a small amount of vaginal estrogen is absorbed if the low-dose estrogen is dosed properly.”
May Protect Against Breast Cancer
The link between breast cancer and hormone therapy (HT) is tricky because there have been studies that have shown estrogen can lower a woman’s risk of breast cancer, but then there are cases where it also increased risk. In addition to that, women who have a history of breast cancer or those who are currently fighting breast cancer are advised against using hormone replacement therapy. We’ve turned to the National Cancer Institute to get to the bottom of breast cancer and hormone therapy.
The source explains that women who took estrogen-only therapy (ET) had a lower risk of breast cancer than those who took the placebo, and their risk remained lower 11 years later during a follow up. However, women who took estrogen plus progestin (EPT) “were more likely to be diagnosed with breast cancer than women who took placebo. The breast cancers in these women were larger and more likely have spread to the lymph nodes by the time they were diagnosed,” writes NIH. “The risk of breast cancer was greater the longer women took the combined hormone therapy, but it decreased markedly when hormone use stopped.”
So while it does reduce the risk, this is only for women who are able to take estrogen-only therapy which is generally only for women who have had their uterus removed.
Cons
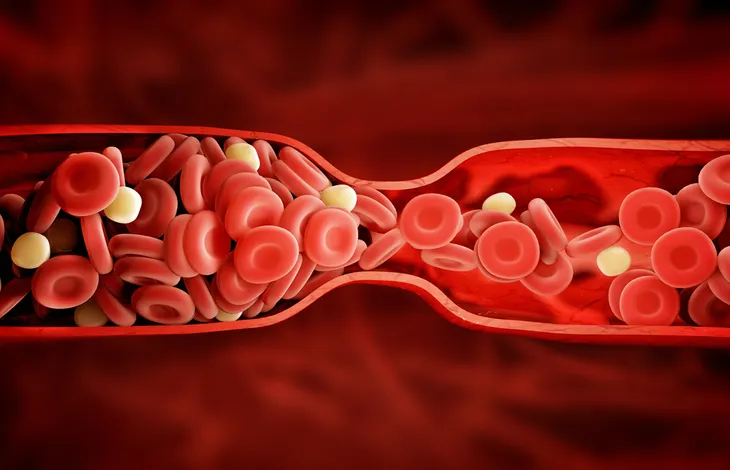
Raise the Risk of Blood Clots, Stroke, and Gallbladder Disease
However, this same study found that estrogen did raise the risk of blood clots, stroke, and gallbladder disease. It also showed “combination therapy also raised the risk of heart attack, breast cancer, gallbladder disease, and death from lung cancer,” writes Healthline.
WebMD also writes that estrogen pills, which is the most common form of estrogen replacement therapy, on their own can cause a slight increased risk of strokes, blood clots, and other problems. When this treatment is combined with hormone progestin, the risk of breast cancer and heart attacks go up as well.
Risky for Women with History of Heart Disease and Cancer
Hormone replacement therapy isn’t meant for everyone. Not only does the risk associated with HRT increase with age, but it can also be dangerous for women who are at an elevated risk for certain health problems. “We worry about women who are at elevated risk of heart disease, have untreated hypertension, atherosclerotic plaque, or are at high risk for dementia or have changes already present in their brain on MRI scans,” says Dr. JoAnn Pinkerton, executive director of the North American Menopause Society and professor of gynecology at the University of Virginia Health System to Healthline. The source also notes that these kinds of risks only increase with the dosage, as well as the longer the medication is taken and as a woman ages.
Another group who should avoid hormone therapy are those who have “previously had breast cancer, ovarian cancer, endometrial cancer, blood clots in the legs or lungs, stroke, liver disease, or unexplained vaginal bleeding should usually not take hormone therapy,” writes the Mayo Clinic. Generally, if your menopause symptoms aren’t bothering you and started after the age of 45, then you do not need to have hormone therapy. When it comes to reducing the risk of osteoporosis and heart disease (which are two of the benefits of HT), there are other treatments available, like medication and lifestyle changes. Always consult with a doctor to make the right decision for you.
Could Cause Liver Problems
Getting hormone treatment through the skin via a patch or gel, could be safer than ingesting it through a pill, says Robin Phillips, a New York gynecologist and editor of “The Menopause Bible: The Complete Practical Guide to Managing Your Menopause” when talking to Healthline. According to Phillips, the pill poses problems for the liver because that is where they are synthesized.
WebMD backs this claim up by stating that people with liver damage should avoid taking any form of oral estrogen. “While estrogen pills can be dangerous for people with liver problems, patches are OK, because the estrogen bypasses the liver and goes directly into the blood,” writes the source. While more studies are needed to draw conclusive results on whether or not the patch is safer than the pill, a 2007 study did find that the patch does not pose the same risk of blood clots that the pill does. Either way, all estrogen prescribed medication still carries a black-box warning informing people of the risk of blood clots.
The source also goes on to note that estrogen could cause problems for people who take certain medication or suffer from stomach problems because, like we mentioned earlier, it’s not always absorbed well. It can also increase cholesterol levels since it’s metabolized in the liver, says WebMD.
Not Recommended for Women Over 60
The time frame and timeline of menopause is different for every woman, but generally, a woman hasn’t entered menopause until she hasn’t had a period for 12 months in a row, explains Healthline. The age that this typically occurs is between 48 and 55. The source goes on to explain that 80-percent of women “experience hot flashes, technically called ‘vasomotor symptoms.’” These vasomotor symptoms were thought to only last anywhere from 6-months to two years, but research shows they can last much longer.
A study published in the JAMA Journal back in 2015 found that “half of all women who experience frequent hot flashes live with them for more than seven years.” Healthline notes that if these hot flashes start while a woman is still bleeding, then it could last even longer.
The Mayo Clinic found that over 40-percent of women aged 60 and up were still experiencing “moderate“ or “severe“ symptoms of menopause. Even though HRT is the most effective treatment for hot flashes, it’s not recommended for older women. “The risks are likely to outweigh the benefits for women starting hormones more than 10 or particularly by 20 years from menopause or over age 60, and certainly started after 70,” says Dr. JoAnn Pinkerton, executive director of the North American Menopause Society and professor of gynecology at the University of Virginia Health System to Healthline.
Be Wary of Long Term Use?
Women should always consult with a doctor before starting hormone replacement therapy to determine whether it is the right choice for them. The Canadian Cancer Society writes that women who are considering HRT need to first talk to their doctor about how severe their menopause symptoms are, individual and family history, as well as how long they should be taking HRT.
“Research shows that long-term use of combined HRT (for 5 or more years) increases the risk of breast and ovarian cancer, heart disease, stroke and pulmonary embolism (blood clots in the lungs),” writes the Canadian Cancer Society. “The research suggests that the risks of long-term combined HRT use outweigh the benefits for most women.”
There are Side Effects
While estrogen pills are well known for their ability to reduce the uncomfortable symptoms of menopause like hot flashes, they can also create new symptoms with their side effects. “Oral estrogen — like any estrogen therapy — can also cause side effects. These include painful and swollen breasts, vaginal discharge, headache, an nausea,” writes WebMD. Some far less common side effects include fluid retention, headaches, skin discoloration, increased breast density which makes mammograms more difficult, and a skin irritation, if using the patch, says Cleveland Clinic.
According to Cleveland Clinic, between 5 and 10-percent of women who go through with hormone replacement therapy experience these side effects, but in most cases they are mild. They are never severe enough that the therapy needs to be stopped. “If you have bothersome side effects from HRT, talk to your doctor. He or she can often reduce these side effects by changing the type and dosage of estrogen and/or progestin,” writes the source.
Certain Treatments Can’t Target Hot Flashes
As you can see, the treatment for menopausal symptoms still has many downfalls and kinks to work out. One of the issues with estrogen treatment in the form of vaginal suppositories, rings, and creams is that it while they are perfect for the vaginal symptoms of menopause like dryness, they won’t help with hot flashes which are another common symptom of menopause.