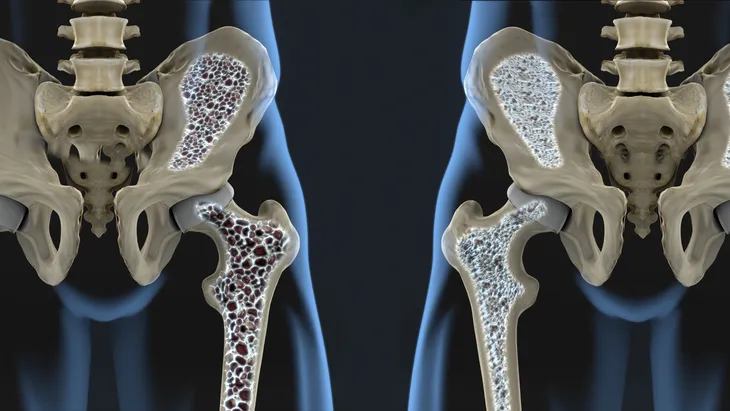
Osteoporosis means “porous bone.” Osteoporosis is a bone disease characterized by the thinning and weakening of bone. The disease affects approximately 8-million women and 2-million men in the United States. Another 34-million Americans have osteopenia, or reduced bone mass, putting them at risk for developing osteoporosis.
A diagnosis of osteoporosis is accompanied by an increased risk of fracturing bones, especially the hip and spine. The United States Preventive Services Task Force recommends screening for osteoporosis in all women 65-years and older with dual energy X-ray absorptiometry (DEXA), also known as a bone density test.
Calcium
Calcium is crucial to humans. It is the most abundant mineral in the body. It is a major component of bones and teeth. Calcium is also needed to help muscles and blood vessels to expand and contract, to secrete hormones and enzymes, and to send messages through the nervous system. Foods rich in calcium include dairy products (cheese, yogurt, and milk) and leafy, green vegetables (turnip greens, kale, bok choy, and broccoli).
A daily intake of 1,200-mg of calcium is recommended for all women diagnosed with osteoporosis. Most women diagnosed with the disease utilize calcium supplements to reach their daily intake goals. The two most common and well-studied calcium supplements are calcium carbonate and calcium citrate. Both are equally well absorbed when taken with food. However, calcium carbonate supplements have the highest percentage of elemental calcium, which translates into fewer tablets to achieve daily intake goals. The most common adverse events reported were constipation and stomach upset.
Vitamin D
Vitamin D is a fat-soluble vitamin. It is essential for strong bones and teeth and helps the body utilize calcium from the diet. The body makes vitamin D when the skin is exposed to sunlight; hence it is often referred to as the “sunshine vitamin.” Most researchers agree 20 to 25-minutes of sunlight per day are helpful. Other sources of vitamin D include fatty fish (salmon, mackerel, trout, tuna, and eel), egg yolks, beef liver, fish liver oils (cod), and fortified dairy and grain products.
The National Osteoporosis Foundation recommends 800 to 1,000-IU of vitamin D daily for persons 50-years and older. Supplements play an important role, because it is difficult to consume that amount of vitamin D through the diet. A study done by the Agency for Healthcare Research and Quality (AHRQ) found daily intake of at least 700 to 800-IU of vitamin D prevented hip fractures in older individuals.
Alendronate
Alendronate (Fosamax) belongs to the group of medicines called bisphosphonates. It inhibits the breakdown of bone by cells called osteoclasts. If these cells are overactive it causes a reduction in bone mass associated with osteoporosis. As a result, alendronate slows bone loss and increases bone mass, which may prevent bone fractures.
Alendronate was the first oral drug approved by the United States Food and Drug Administration (FDA) for the non-hormonal treatment of postmenopausal osteoporosis. It is also used in the treatment of men with osteoporosis and individuals with Paget’s disease of the bone. In a Canadian study, alendronate was shown to increase bone mineral density in the hip and spine. Weekly dosing options exist for alendronate. The drug must be taken with a full glass of water followed by a required 30 to 60-minute wait before reclining or consuming other medications, beverages, or food. The recommendation decreases the risk of upper gastrointestinal adverse effects and helps with absorption.
Risedronate
Risedronate (Actonel) is an oral drug that belongs to the class termed bisphosphonates, which are medications used to treat osteoporosis. A factor in the development of the disease is increased bone breakdown. Risedronate inhibits osteoclasts, which are the cells responsible for the breakdown of bone. It also inhibits the reabsorption of bone. Both measures come together to increase bone density, which is a goal of the treatment of osteoporosis.
Risedronate is approved for the treatment of postmenopausal osteoporosis. It is also indicated for the treatment of male osteoporosis and Paget’s disease of the bone. A study published in the New England Journal of Medicine demonstrated a reduction of hip and spine fractures in individuals with osteoporosis taking risedronate. Weekly and monthly dosing options are available with this drug. Recommendations include taking the drug with a full glass of water followed by a 30 to 60-minute wait before reclining or consuming other medications, beverages, or food.
Ibandronate
Ibandronate (Boniva) is a bisphosphonate approved for the treatment of postmenopausal osteoporosis. The drug’s mechanism of action is inhibition of osteoclasts (cells that break down bone) and bone resorption. The two mechanisms result in an increase in bone mass, which is a goal of the treatment of osteoporosis.
Ibandronate may be administered orally in a monthly dose or intravenously every 3-months. In 2005, ibandronate became the first ever once-monthly oral treatment for any chronic disease. A Danish study found oral ibandronate lowered rates of spine fractures in those with postmenopausal osteoporosis. A Swiss study concluded intravenous dosing of ibandronate was safe and effective in increasing bone mineral density (BMD) in those diagnosed with postmenopausal osteoporosis. Common adverse effects associated with ibandronate are dyspepsia (indigestion), diarrhea, vomiting, and gastritis (inflammation of the stomach).
Zoledronic Acid
Zoledronic acid (Reclast) is a bisphosphonate approved for the treatment of postmenopausal osteoporosis. It also is indicated in the treatment of male osteoporosis and individuals with Paget’s disease of the bone. The drug works by inhibiting the activity of osteoclasts, which are cells that break down bone. It’s the overactive osteoblasts that contributes to the development of osteoporosis. The drug also inhibits the resorption of bone. As a result, zoledronic acid builds bone mass.
Zoledronic acid is administered intravenously in a single dose once a year. A study published in the New England Journal of Medicine found a once-yearly infusion of zoledronic acid during a 3-year period significantly reduced the risk of spine and hip fractures in women with postmenopausal osteoporosis. A Swiss study reported zoledronic acid is the only agent shown to reduce the incidence of fracture and mortality (death) in patients with a previous low-trauma hip fracture.
Raloxifene
Raloxifene (Evista), a selective estrogen receptor modulator (SERM), is approved for the treatment of postmenopausal osteoporosis. The first SERM to come to market was the breast cancer drug tamoxifen. Raloxifene reaps the benefits of estrogen, but without its disadvantages. The drug acts like estrogen on bone by protecting its density. Raloxifene is also indicated to decrease the risk of invasive breast cancer in postmenopausal women with osteoporosis. It also lowers blood concentrations of low-density lipoprotein (LDL), also known as “bad” cholesterol, which is the culprit in atherosclerosis and heart disease.
Raloxifene is prescribed in an oral once-daily dosage. A clinical trial done at Kaiser Permanente concluded raloxifene increased bone mineral density in the spine and hip and reduced the risk of spinal fracture only. The most common adverse effect reported while taking raloxifene was hot flashes.
Calcitonin Nasal Spray
Calcitonin nasal spray (Miacalcin) is approved for the treatment of postmenopausal osteoporosis. It also has indications for the treatment of hypercalcemia (increased levels of calcium in the blood) and Paget’s disease of the bone. For the treatment of postmenopausal osteoporosis, the drug should ideally be administered to women greater than 5-years past menopause. Calcitonin works by inhibiting bone resorption and thus slowing bone loss. Because there are more effective medications available, calcitonin is not used as a first-line agent in the treatment of osteoporosis.
Calcitonin is administered as a nasal spray in a dosage of 200-IU in alternating nostrils each day. A clinical trial from the University of Washington concluded calcitonin nasal spray at a dose of 200-IU daily significantly reduced the risk of new spinal fractures in postmenopausal women with osteoporosis. A study published in Osteoporosis International reported calcitonin had modest pain relieving properties in the setting of acute spinal fractures resulting from postmenopausal osteoporosis.
Teriparatide
Teriparatide (Forteo) is approved for the treatment of postmenopausal osteoporosis. It is the only osteoporosis treatment that increases bone formation. All other osteoporosis therapies work by slowing bone loss. Teriparatide is a synthetic form of the naturally occurring parathyroid hormone, which regulates calcium and phosphate metabolism in bones. Teriparatide is self-administered by subcutaneous injection daily, and can be used for up to 2-years.
A study published in the New England Journal of Medicine found treatment of postmenopausal osteoporosis with teriparatide decreased the risk of spinal and non-spinal fractures. Another study published in the New England Journal of Medicine suggests it is advisable to follow teriparatide therapy with bisphosphonate therapy to maintain increases in bone mass. Reported adverse effects of this agent include orthostatic hypotension (a form of low blood pressure occurring when standing up from sitting or lying down), transient hypercalcemia (elevated blood levels of calcium), nausea, arthralgia (joint pain), and leg cramps.
Estrogen Replacement Therapy
Estrogen replacement therapy (ERT) is widely used to treat symptoms of menopause (estrogen deficiency) such as hot flashes, night sweats, anxiety, irritability, and vaginal dryness, which can lead to dyspareunia, or painful intercourse. In women who have an intact uterus, physicians often prescribe the hormone progesterone in combination with estrogen. The term hormone replacement therapy (HRT) refers to the prescription combination of estrogen and progesterone. The combination reduces a woman’s risk of developing endometrial cancer, which is a cancer involving the lining of the uterus.
Bone loss occurs fastest during and after menopause in response to cessation of estrogen production by the female ovaries. Estrogen replacement therapy halts the bone loss, which prevents the development of osteoporosis. The Women’s Health Initiative (WHI) confirmed that estrogen, with or without progesterone, slightly reduced the risk of hip and spinal fractures. Although HRT is not generally prescribed for osteoporosis, if a woman is taking it for menopause related symptoms, it has the added advantage of helping bone mass.