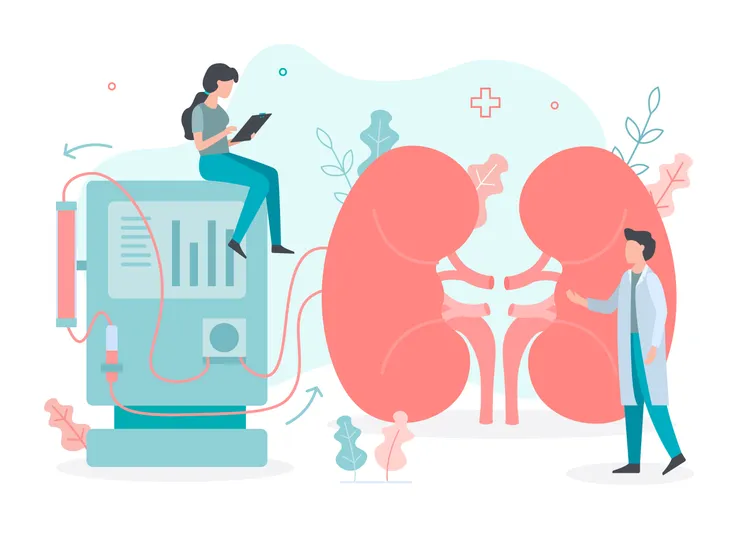
Like most of our organs, our kidneys play an important role in the overall functioning of our body. These two bean-shaped organs sit directly below the rib cage, one on each side of the spine. Their primary job is to remove waste and fluid from the body, says WebMD, but they also maintain blood pressure and mineral levels, keep our bones strong, and help make red blood cells.
A healthy set of kidneys will be able to do all of this for our body, however, people with failing or damaged kidneys might have difficulty eliminating waste from the body or unwanted water from the blood. This is where dialysis comes in.
According to Medical News Today, about 14-percent of the U.S. population has chronic kidney disease (CKD) which means they’ll likely need dialysis. For these people, here’s a look at everything to know about dialysis, including the procedure, types, risks, and overall purpose…
What is Dialysis?
The kidneys perform the important task of cleaning our blood and removing waste and excess fluid from the body. In a healthy person, the kidneys filter around 120 to 150-quarts of blood every day and send excess waste to the bladder so that it can exit the body through our urine, says Healthline. Dialysis is a treatment that uses a machine to mimic the kidney’s job of purifying the blood and keeping the body’s electrolytes in balance.
However, it’s important to note that while dialysis is helpful, it can in no way compare to what the kidneys were able to do when they were healthy, says the American Kidney Fund. A healthy, functioning pair of kidneys are able to remove fluid and waste around the clock, whereas dialysis can only do about 10 to 15-percent of that.
When is Dialysis Needed?
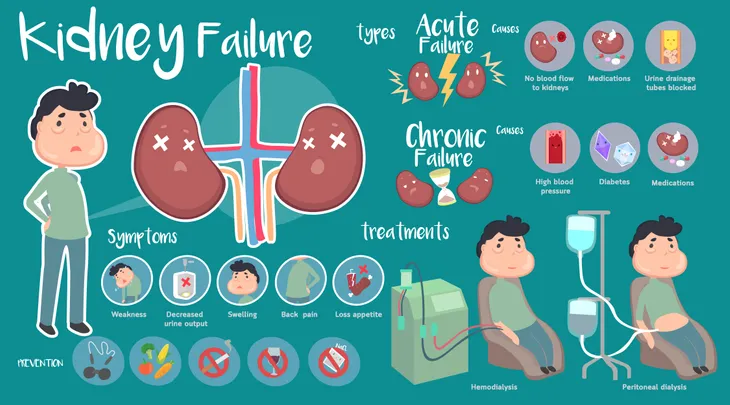
Dialysis is typically used when people are suffering from a severe case of kidney disease or kidney failure, also known as end stage renal disease (ESRD), says the American Kidney Fund. Kidney failure means that the kidneys are no longer taking care of the body’s needs, particularly their job of removing waste and excess fluid.
According to WebMD, dialysis would typically start when a person’s lab tests show toxic levels of waste in their blood. “Symptoms of kidney failure include nausea, fatigue, swelling, and throwing up,” writes the source. Other factors that might come into play are a person’s age, their energy level, overall health, and their willingness to receive treatment.
When the kidneys aren’t working properly, either due to disease or injury, it can put a person’s health at serious risk. If salt and other waste products build up, they can act as poisons that not only affect the body but also can damage other organs and lead to coma and even death, warns Medical News Today. While dialysis isn’t a cure, it can help address these problems.
Types
There are three different types of dialysis: intermittent hemodialysis (IHD), peritoneal dialysis (PD), and continuous renal replacement therapy (CRRT).
The type of dialysis a person receives will depend on their unique situation, the availability of the treatment and cost, explains Medical News Today.
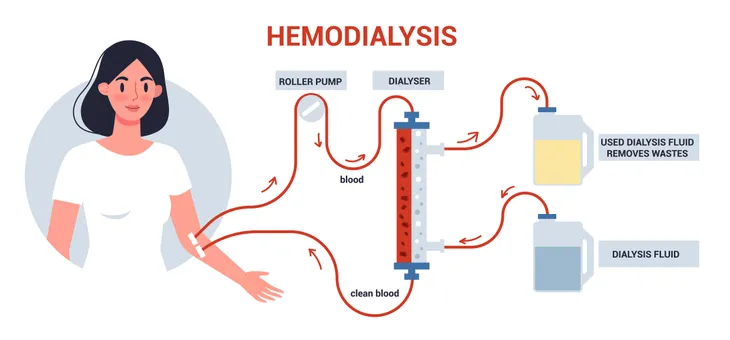
Hemodialysis
Hemodialysis works by using an artificial kidney (hemodialyzer) that removes waste and excess fluid from the blood. In order to access the blood, the patient will have likely undergone minor surgery to create an access point either in their arm or leg, says the National Kidney Foundation. The blood exits their body through a catheter that is inserted into a vein and is filtered through a machine.
This type of dialysis is usually done three times a week for 3 to 4 hours, says Medical News Today. Of course, this can vary depending on how well the kidneys work and how much excess fluid there is between treatments. It can be done at a special center or at home. For those who receive this treatment at home, they’ll need a caregiver who can assist them.
Peritoneal Dialysis
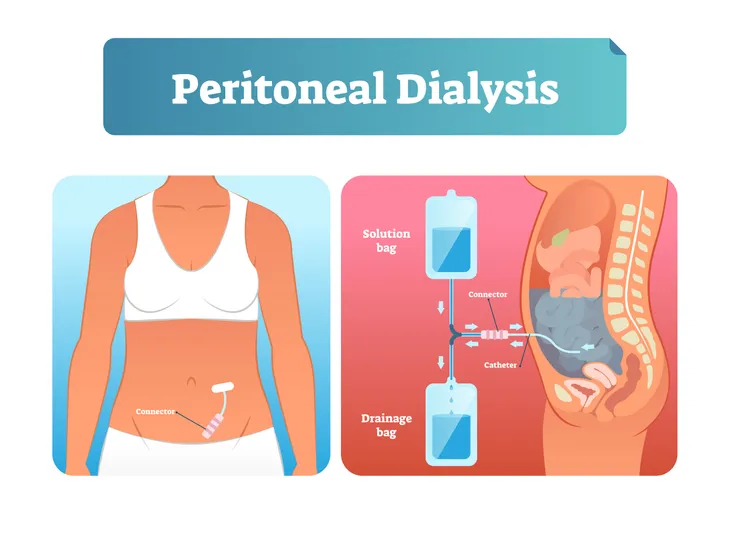
During peritoneal dialysis, the blood is cleaned inside the body. According to the National Kidney Foundation, a doctor will place a catheter inside the abdomen to create an access point. “During the treatment, your abdominal area (called the peritoneal cavity) is slowly filled with dialysate through the catheter,” writes the source. The blood stays in the arteries and veins that line your peritoneal cavity. Any extra waste or fluid is drawn out of the blood and into the dialysate.
There are two types of peritoneal dialysis:
Continuous Ambulatory Peritoneal Dialysis (CAPD): This treatment needs no machinery and can be done by the patient or caregiver. The dialysate is left in the abdomen for 8-hours a day then swapped out for a fresh solution, up to three times a day.
Continuous Cyclic Peritoneal Dialysis (CCPD) or Automated Peritoneal Dialysis: A machine is used to exchange the fluids. It’s generally done at night and each session lasts 10 to 12-hours. Throughout the day, most patients will keep the fluid in their abdomen, but it can be exchanged. This is a good option for people who find hemodialysis too exhausting (i.e., the elderly, children, or infants).
Continuous Renal Replacement Therapy (CRRT)
The last form of dialysis is called continuous renal replacement therapy (CRRT), and just as it sounds, it can be either intermittent or continuous, says Medical News Today. A single session can last up to 6-hours, however, CRRT is often used for 24-hours at a time, such as in an intensive care unit (ICU).
Similar to peritoneal dialysis, there are different types of CRRT. “It can involve either filtration or diffusion. It is better tolerated than intermittent dialysis, because the solute or fluid removal is slower,” writes Medical News Today. This helps reduce the chance of complications and lower the risk of hypotension.
What to Expect
Ahead of your first dialysis treatment, you’ll likely have a tube or device surgically implanted. This provides access to your bloodstream. According to Healthline, it’s a quick operation that doesn’t require a long hospital stay. Most people are able to go home the next day.
During dialysis, you should wear comfortable clothing and follow any instructions from your doctor very carefully. You might need to fast for a period of time before the treatment. It’s also worth noting that dialysis shouldn’t hurt. If you’re experiencing pain after treatment, contact your doctor, says WebMD.
It’s common to feel tired after treatment and have a slight drop in blood pressure, which can cause some nausea, headache, or cramping. These side effects typically go away after several treatments, but if they don’t, talk to your doctor.
What are the Risks?
Dialysis can save a person’s life, but it does come with some risks. Each type of dialysis has its own risks.
Risks of Hemodialysis
The most common risks associated with hemodialysis are…
- Low blood pressure
- Anemia (low red blood cells)
- Muscle cramps
- Difficulty sleeping
- Itching
- High blood potassium levels
- Pericarditis (inflammation of the membrane around the heart)
- Sepsis
- Bacteremia (bloodstream infection)
- Irregular heartbeat
- Sudden cardiac death (the leading cause of death in people undergoing dialysis, says Healthline)
To help lessen these side effects, WebMD suggests closely monitoring food and drink, particularly fluid, protein, and salt. For more information, talk to your doctor.
Risks of Peritoneal Dialysis
For people undergoing peritoneal dialysis, the most common risk is an infection in or around the catheter site in the abdomen. “For example, after catheter implantation, a person can experience peritonitis,” writes Healthline. This is an infection of the membrane lining the abdominal wall.
You might also experience:
- Abdominal muscle weakening
- High blood sugar (a result of dextrose in the dialysate)
- Weight gain
- Hernia
- Fever
- Stomach pain
Risks of CRRT
Healthline lists the following as the most common risks associated with CRRT…
- Infection
- Hypothermia
- Low blood pressure
- Electrolyte disturbances
- Bleeding
- Delayed renal recovery
- Weak bones
- Anaphylaxis
Anyone who continues to experience these side effects should tell the healthcare provider administering the treatment.
Long-Term Outlook
In cases of CKD, the damage is often irreversible, but not all kidney disorders are permanent. Dialysis can sometimes play a role in keeping a person healthy as their kidneys work to repair themselves.
For those that can’t, dialysis is their only option until a kidney transplant becomes available. You’ll also be required to make some lifestyle choices, mainly pertaining to diet. “Your nephrologist (kidney doctor) should have a dietician on their team to help guide dietary choices,” says Healthline.
According to the National Kidney Foundation, for most patients with kidney failure on dialysis, their life expectancy will vary depending on their condition and how well they follow their treatment plan. Most people will live 5 to 10 years, however, many patients have also lived 20 to 30 years.
What If I Want to Stop Dialysis?
While dialysis isn’t a cure by any means, it can greatly improve or sustain a person’s quality of life. However, it’s also a choice, and a person can choose not to undergo dialysis at any time. WebMD points out that anyone who is considering stopping their dialysis treatment should talk to their doctor and explore other potential treatments that can help. There are some lifestyle choices that can help.
If you’re wanting to stop dialysis due to shame or embarrassment, talk to your doctor. They might encourage you to speak to a counselor first, says WebMD. “Sharing your feelings, taking antidepressants, or doing both of these things may help you make a more informed decision,” writes the source.
Undergoing dialysis is a major commitment and it’s not for everyone. It can be particularly hard for the elderly or those with severe medical conditions.