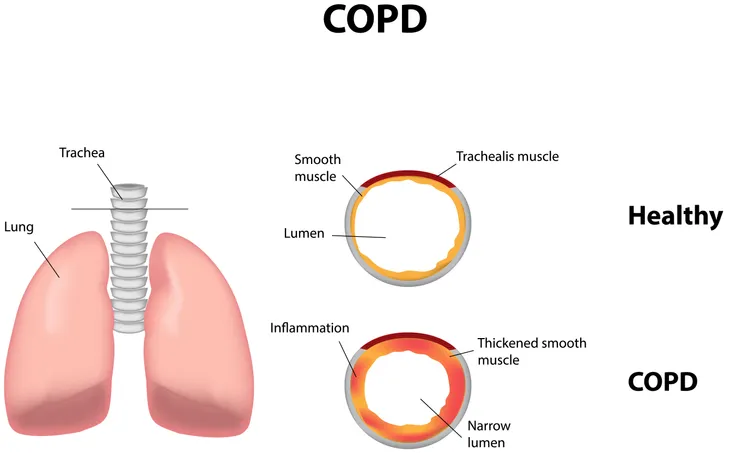
Chronic obstructive pulmonary disease (COPD) is a chronic inflammatory lung disease where the airways in the lungs become swollen and partly blocked. While COPD is treatable, if left untreated it can progress over time and lead to more serious complications like heart disease, lung cancer, and a variety of other infections and conditions.
Exposure to COPD triggers, known or unknown, can contribute to the progression of COPD. While triggers can change from person to person, to help minimize your exposure to COPD flare-ups or potentially even avoid getting COPD in the first place, continue reading to learn the most common COPD triggers.
Main Categories of Triggers
The most common COPD triggers belong to three main categories:
- Air Pollution and Irritants
- Weather
- Respiratory Infection
Air Pollution and Irritants
Cigarette Smoke
Inhaling cigarette smoke, either as a result of you smoking or secondhand smoke from someone around you is responsible for at least 85-percent of all cases of COPD. The damaging effects of smoking are well known, but the tar and many other toxic chemicals inside cigarettes damage the lungs by causing inflammation, destroying the air sacs, and narrowing the air passages. If you already have COPD, inhaling cigarette smoke can also worsen your symptoms and increase your risk of lung infection.
If you currently smoke, to avoid the onset or progression of COPD (among other negative effects), you should quit immediately. Otherwise, try to distance yourself from secondhand smoke as much as possible.
Indoor Fumes and Irritants
Various cleaning products, paints, and fume-containing solvents can also trigger COPD exacerbations. In fact, in a 2015 study that included 167 people with COPD, more than half the participants reported that performing household chores involving certain chemicals made their symptoms worse.
These chores involved such chemicals as:
- Cleaning products
- Perfumes
- Scented products, such as candles, bug spray, and hair products
- Wood smoke
In the same 2015 study, dust and pet dander were also found to be major triggers while performing household chores, such as sweeping, dusting, and vacuuming. Add on fumes and odors caused by cooking, fireplaces, and kerosene heaters, as well as dirty air filters, and your home can become a breeding ground for COPD irritants.
To avoid these triggers, when cooking or cleaning, work in a well-ventilated area, use natural cleaning products without harmful irritants, take regular breaks, and consider wearing a protective mask in some cases. Vacuuming more often, hardwood floors, and restricting pet access around the house can all also help avoid COPD flare-ups.
Outdoor Fumes and Irritants
Outside of your home, there are other chemical fumes that can irritate COPD. These include:
- Vehicle exhaust
- Factory pollution
- Spills at gas stations
- Sewer fumes
- Pollen
If you have to be outside around heavy amounts of any of the above, you should limit any outdoor activities that require you to breathe more air than usual (such as exercise). This is especially true when smog levels are high, as there is data to suggest that high levels of ozone in the air may cause COPD flare-ups.
Fortunately, in most cases, you can get ozone readings simply by checking your local weather channel. As a rule of thumb, ozone levels tend to be at their highest between May and September and are higher in the afternoon than they are in the morning.
Staying inside during high smog levels, avoiding obvious pollutants, and, in some cases, wearing a painter’s mask outside can all help reduce the risk of your COPD flaring up.
Weather
In 2017, a study consisting of 106 people with COPD recording their symptoms, the humidity level, and the temperature each day for over a year, found that the combination of low temperature and high humidity was likely to trigger COPD symptoms.
In response, researchers recommended people with COPD keep their indoor temperatures at 18.2°C (64.8°F) or above to ensure a humidity level of 70-percent or less. Ideally, indoor air humidity should be at 40-percent. This can be more easily achieved with the help of a dehumidifier.
Along the same line, people with COPD should also limit time outdoors during extremely hot (above 90°F [32°C], cold (below freezing), windy, or humid weather. During cold weather, if you have to go outdoors, covering up your mouth and nose as best as possible is recommended. On very hot and humid days, frequent breaks inside, preferably with air conditioning, is the best way to avoid COPD flare-ups.
In fact, it’s not uncommon for people with more serious cases of COPD to move to other parts of the country (or world) where weather conditions are more COPD-friendly.
Respiratory infections
While not necessarily a trigger for COPD, because COPD damages the lungs, it increases the risk of contracting respiratory infections, such as colds, the flu, and, if left untreated, even pneumonia. The combination of these issues is also more likely to become severe and lead to complications.
This is because many of the symptoms of more common respiratory infections can make COPD symptoms worse, including
- Coughing
- Wheezing
- Shortness of breath
- Fatigue
Prevention
Because of this, the Centers for Disease Control and Prevention (CDC) recommend that people with COPD get vaccinated against pneumococcal diseases and receive an annual flu shot. As recommended by your doctor, other vaccinations may be required.
Other than getting vaccinated, the Cleveland Clinic also recommends that people with COPD:
- Stay hydrated
- Practice good hygiene
- Keep your home sanitized
- Avoid crowded places and people who are sick to reduce your risk of getting an infection
In the case that you do get infected, it’s important to seek professional attention as soon as possible to avoid your COPD or infection getting any worse.