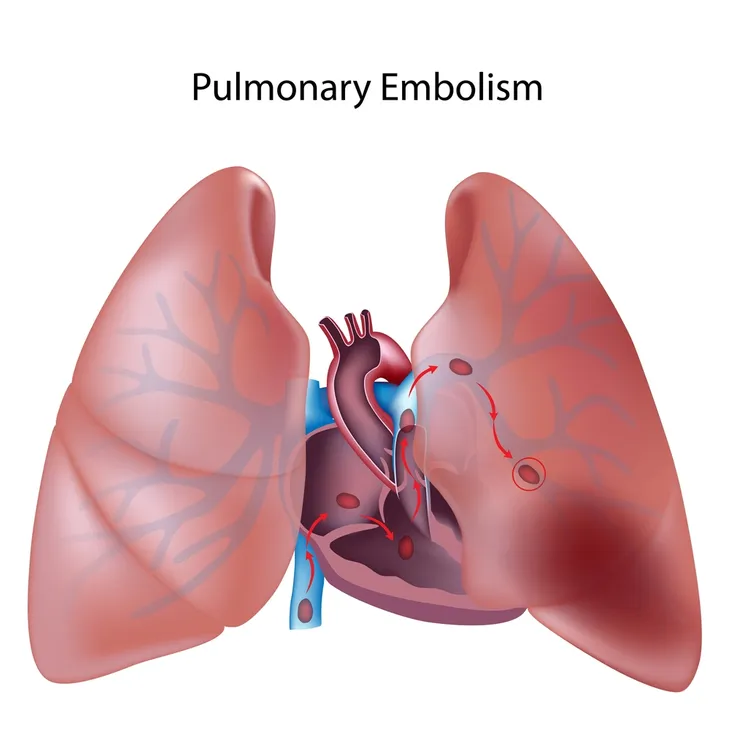
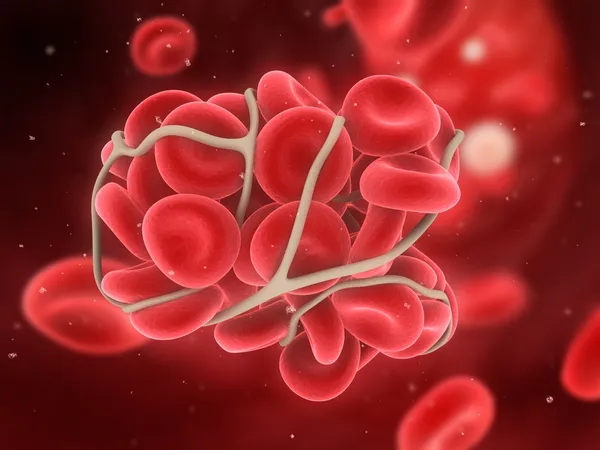
A pulmonary embolism (PE) occurs when a blood clot gets caught in one or more of the pulmonary arteries which is where blood travels from the heart to the lungs. These clots can start in the lungs or have traveled into the lungs from elsewhere in the body, like a deep vein in the legs. Either way, when a clot ends up here, it can be fatal.
These clots are so dangerous because they have the potential to damage the lungs and impact oxygen levels in the blood which affects other organs in the body. There are several telltale symptoms and certain risk factors we should all be aware of to protect ourselves. In this article, we’re going to cover all the symptoms, causes, and treatments of a pulmonary embolism…
1. What Is It?
Healthline notes that a PE refers to a blood clot that occurs in the lungs. The result is possible lung damage due to limited blood flow, as well as decreased oxygen levels in the blood. A PE may impact certain other organs as well, it adds.
The problem can be life threatening, and can even lead to death. “It results in the death of one-third of people who go undiagnosed or untreated,” writes Healthline while citing the Mayo Clinic. “However, immediate emergency treatment greatly increases your chances of avoiding permanent lung damage.”
2. Most Common Symptoms
While there could be a long list of associated symptoms, usually three of them seem to be the most prominent, according to the Mayo Clinic. The common symptoms are shortness of breath, chest pain, and a cough (which may include traces of blood).
“Pulmonary embolism symptoms can vary greatly, depending on how much of your lung is involved, the size of the clots, and whether you have underlying lung or heart disease,” adds the clinic.
3. Other Telltale Symptoms
The Mayo Clinic notes that on top of the three main symptoms, there are other possible symptoms of a PE. These symptoms can include clammy or discolored skin (medically known as cyanosis), fever, or a rapid or irregular heartbeat.
You may also experience leg pain and swelling (usually in the calf), excessive sweating (sometimes referred to as hyperhidrosis), or even lightheadedness or dizziness.
4. Causes of a Pulmonary Embolism
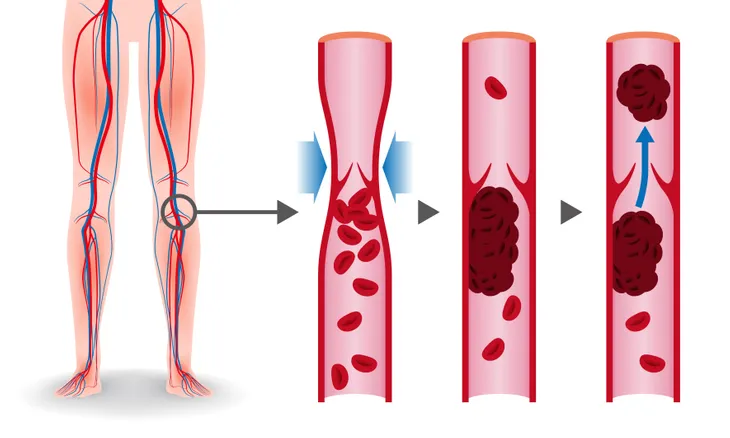
WebMD says the main cause of a PE is a clot in the lower part of the leg or thigh called deep vein thrombosis (DVT). “[PE] usually travel to the lungs from a deep vein in the legs,” explains the source.
Meanwhile, the cause of DVT is usually due to long periods of inactivity, such as when you’re on a long plane ride or you’re on bed rest following a medical procedure, it adds.
5. Other Risk Factors
Other reasons you might develop a PE include increased clotting of your blood, known medically as hypercoagulability, according to WebMD. This can be caused by certain medications, such as birth control pills.
Other risk factors include smoking, being pregnant, or having damage to a blood vessel wall. “Trauma to your lower leg can lead to this,” notes the source. These additional risk factors together are known in the medical world as “Virchow’s triad,” says WebMD.
6. Medical History Factors
The Mayo Clinic explains that having certain underlying medical conditions or undergoing medical procedures can increase your likelihood of developing a PE as well. These include heart disease that can make “clot formation more likely,” cancer, or surgery, although medications are sometimes given before and after procedures to avoid the problem.
Genetics can also play a part in your risk level. “You’re at higher risk if you or any of your family members have had venous blood clots or pulmonary embolism in the past,” explains the clinic.
7. How is it Diagnosed?
WebMD says if you have any telltale signs of a PE, you should get medical help immediately. A doctor will usually begin with a physical exam, looking closely at your legs for swelling or tenderness.
Next, focusing more on the upper body, your doctor may also order a chest X-ray and computed tomographic angiography (CTA) that can visualize blood vessels in your lungs with the help of dye injected into the veins. If you’re pregnant, a magnetic resonance imaging (MRI) scan may be used as an alternative.
8. Possible Complications of a Pulmonary Embolism
The Mayo Clinic warns that approximately 33-percent of patients that have an untreated PE die as a result. “When the condition is diagnosed and treated promptly, however, that number drops dramatically,” adds the clinic.
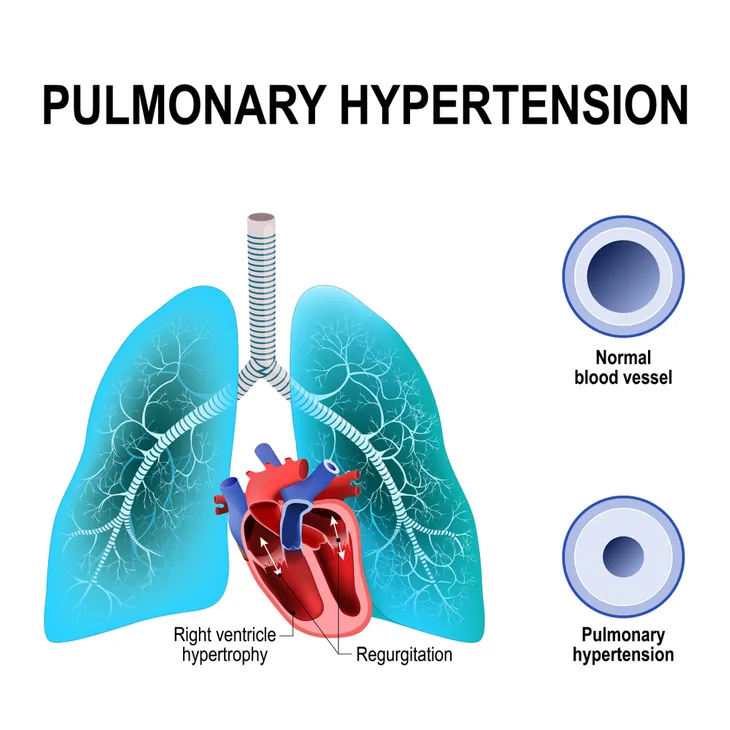
A PE can also cause pulmonary hypertension, which causes blood pressure in your lungs and the right side of your heart to rise to abnormal levels. “When you have obstructions in the arteries inside your lungs, your heart must work harder to push blood through those vessels,” notes the clinic. This increased blood pressure can ultimately weaken your heart.
9. Avoiding a Pulmonary Embolism
The National Heart, Lung, and Blood Institute has some tips for avoiding a venous thromboembolism (VTE), which includes PE. To help prevent a “first VTE event,” movement is the primary approach. “Helping your blood circulate makes it harder for clots to form,” notes the source.
If you’re at risk or are going in for surgery, gentle pressure is another way to keep blood from pooling and clotting. Compression stockings may be a way to achieve this. Doctors may also prescribe blood thinners and other medications to keep your blood from clotting before or after surgery.
10. Treatment
The Cleveland Clinic explains a PE is generally treated in a hospital with close monitoring. In any case, doctors may turn to anticoagulant (blood thinner) medications or thrombolytic therapy, which refers to clot busting medications.
If the clot is life-threatening or if other treatments are not proving to be effective, you might require surgery to remove the clot from the pulmonary artery. There’s also an “interventional procedure” that places a filter inside the vena cava (your largest vein) to trap clots before they can enter the lungs.
11. Ongoing Care
If you’ve been put on blood thinners, you may be called back for blood tests to monitor their effectiveness and to measure how long it takes for your blood to clot, adds the Cleveland Clinic.
Compression stockings are also often prescribed by doctors to assist with blood flow in the legs and prevent pooling of blood. “Talk with your doctor about how to use your compression stockings, for how long, and how to care for them,” suggests the clinic.
12. Keep Moving
As we mentioned before, being still for long periods of time (for example, while traveling in a plane or car) can add to the risk factor of developing a blood clot.
However, The Guardian points to a study that shows a sedentary lifestyle namely a lifestyle without regular activity can lead to a PE. The study focused on about 70,000 nurses in the U.S. While nurses are often constantly on their feet while working, “the researchers found that those who sat for longer than six hours a day when they were not working had twice the risk of a [PE] than those who sat for less than two hours a day,” notes the source.