The gallbladder is a little pear-shaped pouch located behind the liver that has a not-so-little job. This organ is responsible for storing bile (and other fluids), the fluid our body uses to break down fats and digest food. Unfortunately, it’s not uncommon for people to have issues with their gallbladder, including gallbladder disease.
A person may develop gallbladder disease from too much cholesterol or bilirubin in the bile which can lead to gallstones, acute or chronic inflammation, or bile duct stones. These can all cause uncomfortable symptoms that may lead to either open or laparoscopic gallbladder removal surgery. Here are 20 things you should know about the procedure and what to expect afterwards…
1. Function of the Gallbladder
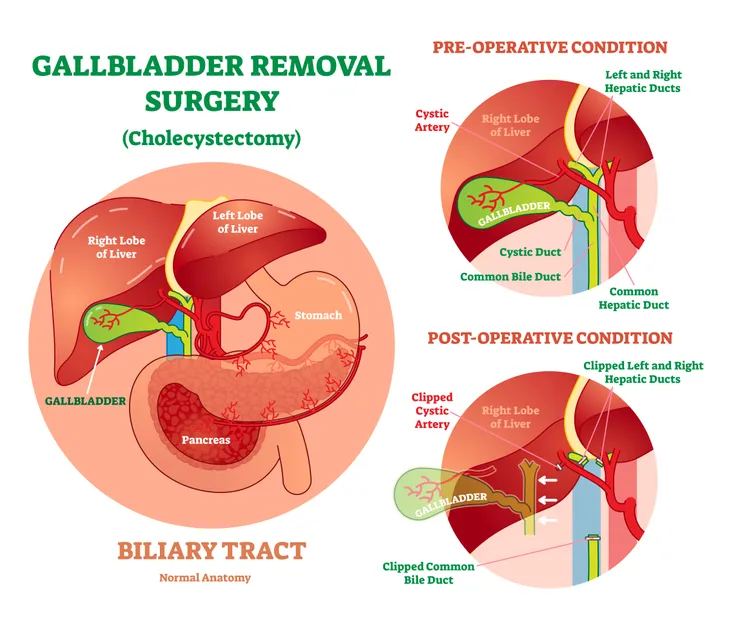
Healthline says although the gallbladder is not essential to live, it does perform a rather important function. The tiny digestive organ sits alongside your liver, connected to it via the “common bile duct.”
“This duct transports bile from the liver through the hepatic ducts, into the gallbladder, and into the duodenum – the first part of your small intestine,” it adds. In short, your gallbladder is a storage facility for bile, and without it, it’s a bit more difficult for your body to break down fatty or high-fiber foods, notes the source.
2. Why Remove the Gallbladder?
Healthline.com explains that you’ll need your gallbladder removed if you “have a tendency to develop painful gallstones,” which are hard deposits usually made of cholesterol but can also contain calcium salts and other bodily fluids.
These gallstones can block the bile ducts from the gallbladder or liver, which can cause infection and pain. It can also interfere with your pancreas, leading to pancreatitis.
3. Causes of Gallbladder Issues
There are multiple reasons that you could experience gallbladder issues. Statistically, patients are more likely to struggle with gallbladder problems if they are female, have had children, are overweight, and/or are over the age of 40. Another common cause of gallbladder issues is genetics.
4. Symptoms of Gallbladder Issues
There are a few key indicators of gallbladder issues that are important to keep an eye out for, which could ultimately lead to having to undergo a gallbladder removal surgery. A few common symptoms of gallbladder problems include sharp pain in the abdomen, nausea, vomiting, indigestion, fever, and jaundice.
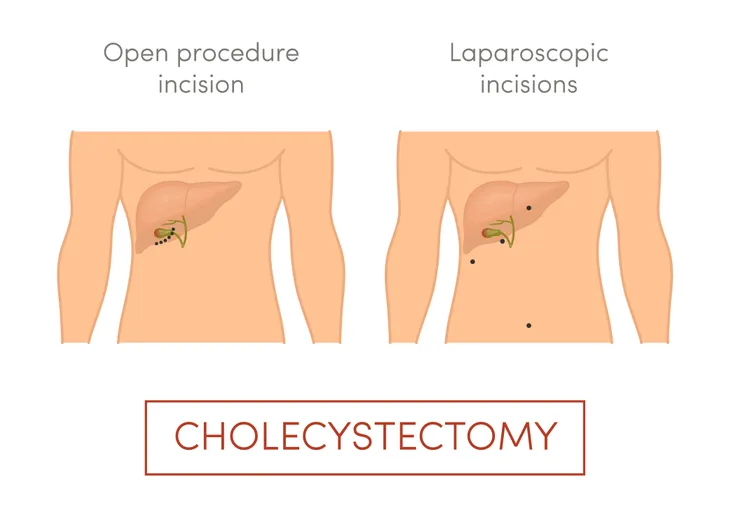
5. Cholecystectomy is the Gallbladder Removal Medical Term
If you begin experiencing gallbladder issues such as gallstones, or other problems, you may need to have your gallbladder removed.
The official medical term for gallbladder removal surgery is a “cholecystectomy.” According to HealthGrades.com, the surgery is typically performed under general anesthesia, so the patient will be asleep during the procedure.
6. How Common is the Surgery?
If you’re feeling nervous about having your gallbladder removed, know that it’s “one of the most common general surgery procedures in the country,” as well as one of the safest, according to Prevention.
The chances of complications during gallbladder removal surgery are less than 5-percent, and most of them will be “non-serious issues” such as minor bleeding.
7. Preoperative Evaluations And Blood Tests Will Occur
It’s likely that your doctor will request a diagnostic test before deciding whether you need a cholecystectomy. Often these tests will include blood tests and x-rays. Another common preoperative test is an ultrasound or a HIDA scan which uses an injection of dye to show how well your gallbladder and bile duct is working.
8. General Surgeons Perform Most Gallbladder Surgeries
According to HealthGrades.com, a cholecystectomy is a surgery that will be done by a general surgical team in a hospital or surgery center. It’s likely the lead surgeon on this team will be either an endoscopic surgeon, a gastrointestinal surgeon, or oftentimes a general surgeon. All of the outlined surgeons will be qualified to perform a gallbladder removal procedure.
9. How To Prepare For Surgery
There are a few ways to prepare for a cholecystectomy which will be outlined by your doctor. The exact instructions on how to prepare will be up to your doctor, however, there are a couple of common guidelines you can follow.
It’s often recommended to take a shower the night before your surgery or the morning before and your surgeon may request you to use antibacterial soap. The doctor will also outline a time to stop eating and drinking leading up to the surgery. Your doctor might also prescribe certain medications to take before surgery which could include blood thinners or supplements.
10. Removal Method: Open Cholecystectomy
MedicineNet.com explains this type of surgery has been used for more than 100-years and is a “safe and effective method for treating symptomatic gallstones, ones that are causing significant symptoms.”
A cholecystectomy is the removal of gallbladder through a 5 to 8-inch incision in your abdomen. “During an open cholecystectomy, the cut is made just below your ribs on the right side and goes to just below your waist,” it adds.
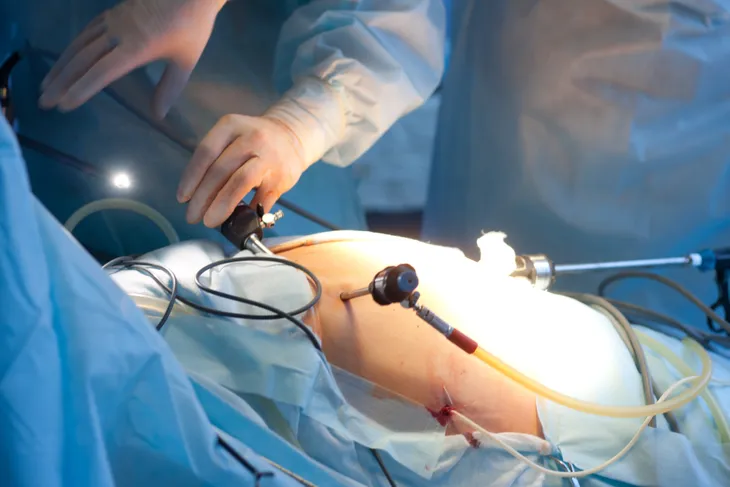
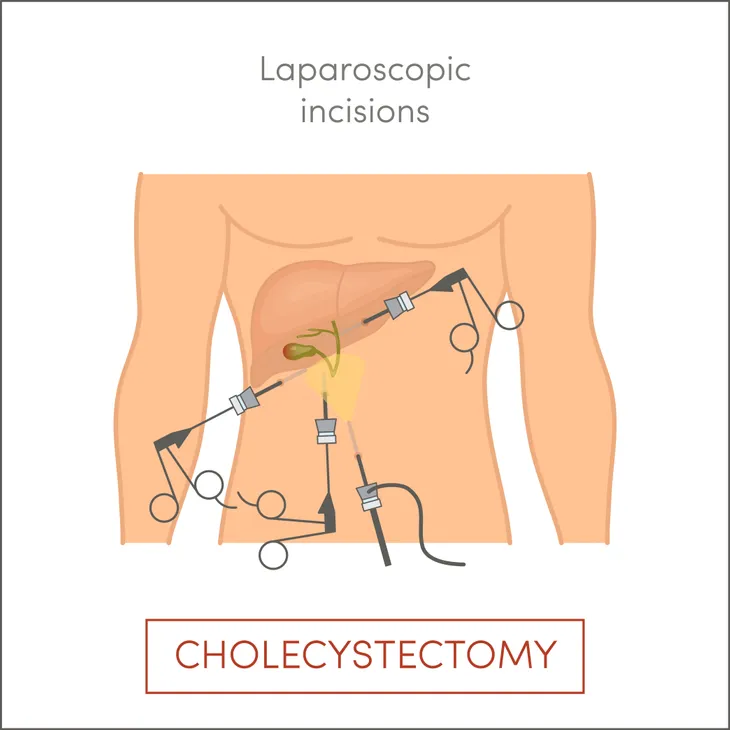
11. Removal Method: Laparoscopic Cholecystectomy
MedicineNet.com explains this common method of gallbladder removal is less invasive, using a laparoscope to do the work. This instrument lets doctors see inside your body, and the surgery is performed “through several small incisions rather than through one large incision,” it adds.
During a laparoscopic cholecystectomy procedure, there are usually four incisions involved, all of them 1-inch or less. The open method may be used if the gallbladder is too inflamed to remove through a small incision.
12. Recovery Time: Open Cholecystectomy
In the case of this open procedure, which is actually less used than the laparoscopic method these days according to SELF, you may have to stay in the hospital for a week or so. In addition, you may have to avoid strenuous activity for up to 1-month.
This method usually requires more pain management, and there could be some “dark bloody fluid” leaking from the incision, which is normal according to the source. You may also have tubes inserted to help remove these fluids as you heal, which will typically come out 2 to 4-weeks following the procedure. Full recovery can take up to 8-weeks, says the source.
13. Recovery Time: Laparoscopic Cholecystectomy
Because this procedure is less invasive, you can expect to be back on your feet and back to your regular routine quicker than the open method, says Self. “Most people who get a laparoscopic cholecystectomy get discharged on the same day and can resume normal physical activity after a week,” it says.
However, you may experience some “residual pain” as well as a sore throat from the breathing tube, warns the source. You may also experience some nausea or vomiting and bruising around the incisions, it adds. “Overall, full recovery takes about one to three weeks,” it offers.
14. Risks of Gallbladder Removal: Infection
As we stated earlier, complications from gallbladder surgery aren’t very common at all, but the surgery itself is. That being said, it’s not completely without risks.
The NHS in the UK explains there’s a chance of wound infection, bile leaking into the stomach, or damage to a bile duct from the liver.
15. Risks of Gallbladder Removal: Bleeding & Blood Clots
While highly uncommon, another risk of gallbladder removal is bleeding or blood clots. Patients with certain risk factors such as prior blood clots, prolonged immobilization, or cancer are at higher risk for developing these issues after surgery.
If you fall in the category of high risk for blood clots, you may need to wear a compression stocking post-surgery to prevent clots from forming in the legs.
16. Information to Digest
While your body will still be able to break down foods, you may have to make some modifications to aid in the process, explains Everyday Health. Instead of bile being stored, it is constantly being dumped into your intestine. “In theory, this means that you will not digest food as well,” it says.
That means for the first 3-weeks or so following surgery, your doctor will likely recommend you stick to a low-fat diet to let your body adapt to the changes, adds the source, which notes 90-percent of patients “go back to eating the way they did before.”
17. Your Stool May Change
Prevention explains the change in the bile mixture may result in some unusual stools – at least compared to what you had before gallbladder removal surgery.
“So if you eat a high-fat meal, your poop might be a bit looser – and this may be the case for life,” explains the source. This also means you may need to stay closer to a bathroom if you plan to indulge in some greasy fast food, it adds.
18. Managing Digestive Problems
You may have some ongoing digestive issues after your gallbladder has been plucked from your body, but they are manageable, notes Everyday Health. For example, you may need to take certain medications that bind to bile, it explains.
There are also some lifestyle changes you can make, such as adopting a low-fat diet (permanently), avoiding fried foods, eating smaller but more frequent meals, and avoiding eating a large meal after fasting for the day, adds the source.
19. You May Not Miss it At All
Prevention says you’ll “have no clue you’re sans gallbladder,” and you won’t get any “phantom pains,” as you might if you had a limb amputated.
Patients on the site report functioning “perfectly fine” without the gallbladder and without any long-term complications. The bottom line is that you more than likely won’t be regretting the surgery that rids you of pain from an inflamed organ.
20. Call Your Doctor If You Experience Complications
While complications are highly unlikely with gallbladder removal surgery, it’s recommended that you contact your doctor immediately if you notice any concerns. A few immediate causes of concern include fainting, shortness of breath, signs of infection, or signs of a blood clot.