Women who are pregnant can become infected with same STIs as women who are not pregnant. Many women with STIs have no symptoms and are unaware they are infected. Pregnant women should be tested for STIs, because infection can have potentially serious consequences for a woman and her baby. Many of the STIs that can be contracted during pregnancy are treatable. Ten sexually transmitted infections that can affect pregnancy are…
1. Chlamydia
Chlamydia is the most common bacterial STI in the United States. The bacteria Chlamydia trachomatis causes the infection. Women with an infection may experience abnormal vaginal discharge, bleeding after sex, or burning with urination. Many women experience no symptoms. An untreated chlamydia infection can lead to complications such as pelvic inflammatory disease (PID), ectopic pregnancy (a pregnancy outside of the uterus), and infertility.
All pregnant women should be tested for chlamydia with the nucleic acid amplification test (NAAT). The test may be done using a urine sample. Chlamydia can be treated with appropriate oral antibiotics. Untreated chlamydia infection in pregnant women has been associated with miscarriages, low birth weight (infant being born weighing less than 5-pounds 8-ounces), and premature (early) birth. A newborn may become infected as it passes through the birth canal. Mother-to-child transmission of chlamydia can cause pneumonia and serious eye infections that may lead to blindness.
2. Human Immunodeficiency Virus
Human immunodeficiency virus (HIV) attacks the immune system. It destroys a type of white blood cell called a helper T-cell, which is also referred to as a CD4 cell. The two main types are HIV-1 and HIV-2. HIV-1 is the most common type. If left untreated, HIV can lead to acquired immune deficiency syndrome (AIDS), which can be fatal. AIDS is clinically defined by a CD4 cell count of less than 200.
HIV testing is recommended for all pregnant women. A blood test is done to detect any antibodies against HIV. Positive test results are confirmed with a Western blot blood test. Mothers can be treated with highly active antiretroviral therapy (HAART) to control their infection and significantly reduce the risk of transmission to the fetus. With HAART, the risk of mother-to-child transmission of HIV can be lowered to less than 2-percent.
3. Gonorrhea
Gonorrhea, also called the “clap” or “drip,” is a very common STI and caused by the bacteria Neisseria gonorrhoeae. Women with an infection may experience abnormal vaginal discharge, lower abdominal or pelvic pain, burning with urination, bleeding after sex, or bleeding between periods. Many women experience no symptoms. An untreated gonorrhea infection can lead to complications such pelvic inflammatory disease (PID), ectopic pregnancy (a pregnancy outside of the uterus), and infertility.
All pregnant women should be tested for gonorrhea, which can be accomplished by using a nucleic acid amplification test (NAAT) on a urine specimen. Gonorrhea may be treated with appropriate antibiotics orally or by injection. Untreated gonorrhea during pregnancy has been associated with miscarriages, premature (early) birth, and low birth weight (infant being born weighing less than 5-pounds 8-ounces). A newborn may become infected as it passes through the birth canal. Mother-to-child transmission of gonorrhea may lead to life-threatening blood infections and serious eye infections that may lead to blindness.
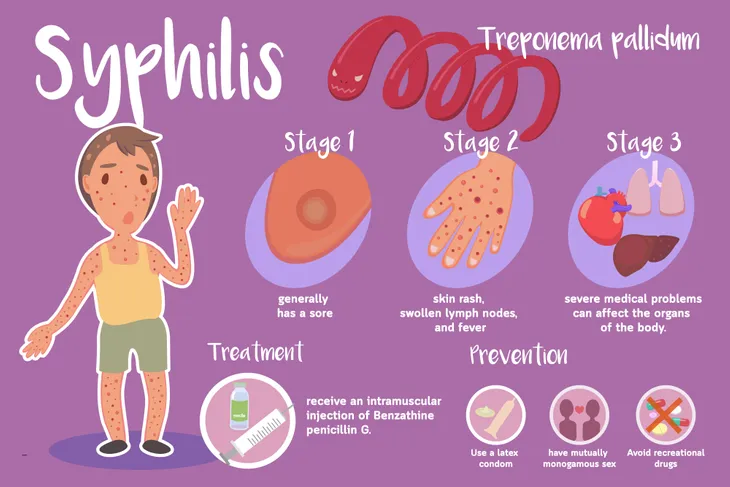
4. Syphilis
Syphilis is caused by the bacteria Treponema pallidum. Syphilis has three stages. The first (primary) stage involves the formation of a chancre, a non-painful ulcer, and lasts 1 to 5-weeks. The second (secondary) stage may include swollen lymph nodes, hair loss, sore throat, fever, and a skin rash involving the palms of the hands. It can last 4 to 6-weeks. The third (tertiary) stage involves the brain and heart and can lead to death.
All pregnant women should be tested for syphilis with either the rapid plasma reagin (RPR) or Venereal Disease Research Laboratory (VDRL) blood test. Syphilis may be treated with penicillin G (an antibiotic) injections. Syphilis has been linked to miscarriages and premature (early) birth. Passing syphilis on to an unborn baby can lead to serious health problems in multiple organs (including the brain, eyes, ears, heart, skin, teeth, and bones) and even death.
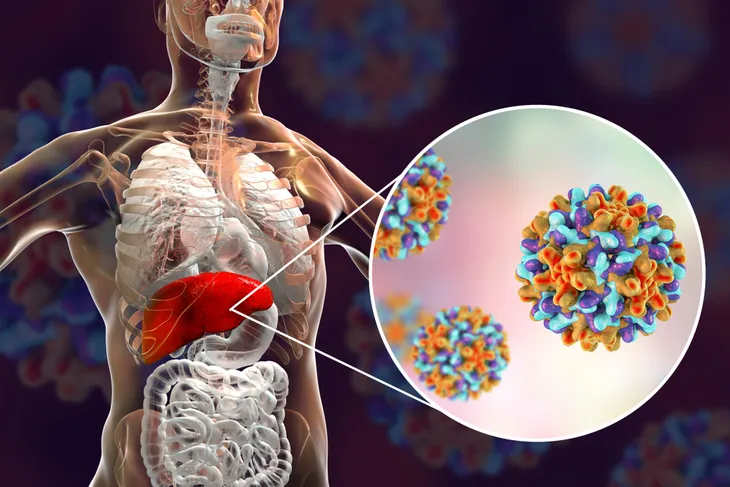
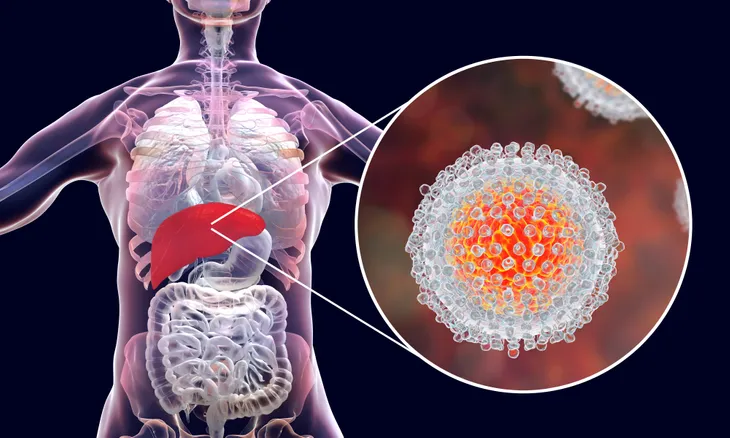
5. Hepatitis B
Hepatitis B is a liver infection caused by the hepatitis B virus. The infection can be acute (short-lived) as well as chronic (lifelong). An acute hepatitis B infection may cause symptoms such as yellowing of the skin and eyes (jaundice), dark urine, extreme fatigue, nausea, vomiting, and abdominal pain that last several weeks. Most people do not experience any symptoms during the acute infection phase. In some people, the infection can become chronic and progress to liver cirrhosis or liver cancer.
Hepatitis B testing is recommended for all pregnant women using a blood test for hepatitis B surface antigen (HbsAg). If a pregnant woman is infected with hepatitis B, she can transmit the infection to her baby through the placenta approximately 40-percent of the time. Infected newborns have an almost 90-percent chance of developing chronic hepatitis B. Currently, there is no cure for chronic hepatitis B, but it is preventable through vaccinations.
6. Genital Herpes
Genital herpes is one of the most common STIs in the United States. It is caused by the herpes simplex virus, which has two specific types: herpes simplex virus 1 (HSV-1) and herpes simplex virus 2 (HSV-2). Both types of HSV can cause genital herpes. Most individuals with genital herpes are unaware they are infected. When present, symptoms may include itching, pain, blisters, or sores in the genital area. The blisters rupture and eventually become scabs, which resolve over a few weeks.
Routine testing for genital herpes is not recommended in pregnant women. If blisters or sores are present, taking a sample for examination in the laboratory can provide a diagnosis. There is no cure for genital herpes, because the virus lies dormant in the nerves and can reoccur at any time. Antiviral medication can help an initial outbreak heal swiftly. Antiviral medications can also be used to reduce the frequency, severity, and duration of recurrent outbreaks. Mother-to-child transmission is rare, because birth by C-section is recommended for all women in labor with active genital herpes.
7. Hepatitis C
Hepatitis C is a liver infection caused by the hepatitis C virus. The infection can be acute (short-lived) as well as chronic (lifelong). Individuals with an acute hepatitis C infection do not typically experience symptoms. Between 15 and 45-percent of infected individuals will have resolution of the acute disease within 6-months. The remaining 55 to 85-percent of infected individuals will develop chronic disease. Chronic hepatitis C infection increases the risk of developing liver cirrhosis and liver cancer.
Routine blood testing for hepatitis C in pregnant women is not recommended. Pregnant women with risk factors such as a history of injection drug use, blood transfusion or organ transplantation before 1992 should be offered testing. A pregnant woman infected with hepatitis C has a 5-percent chance of transmitting it to her baby. Breastfeeding does not transmit hepatitis C. Treatment with antiviral medication can cure the disease. Currently, there are no available vaccines for the prevention of hepatitis C.
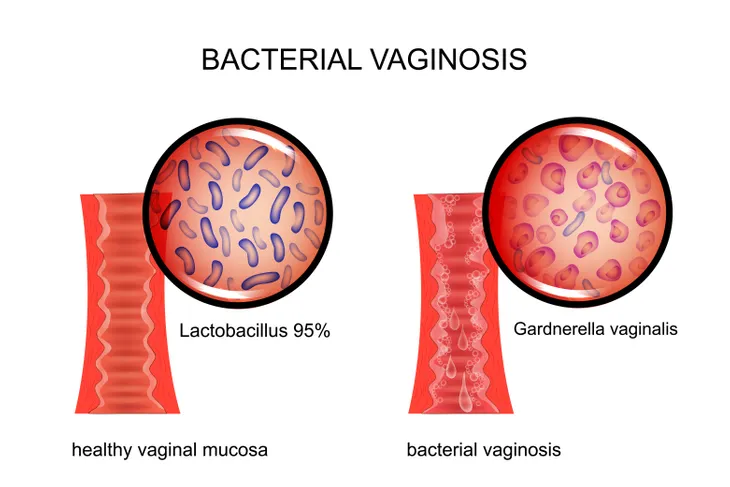
8. Bacterial Vaginosis
Bacterial vaginosis (BV) is often not considered an STI, but it is more common in sexually active women. Having BV may increase a woman’s chances of contracting an STI. Bacterial vaginosis represents an overgrowth of nonbeneficial bacteria in the vagina. Women may complain of a foul-smelling, fishy, vaginal discharge. Many women may have no symptoms.
Testing all pregnant women for bacterial vaginosis is not currently recommended. It may be diagnosed by analyzing a sample of vaginal fluid. The infection may be treated using appropriate oral antibiotics. Bacterial vaginosis during pregnancy has been linked to premature (early) birth and low birth weight (infant being born weighing less than 5-pounds 8-ounces).
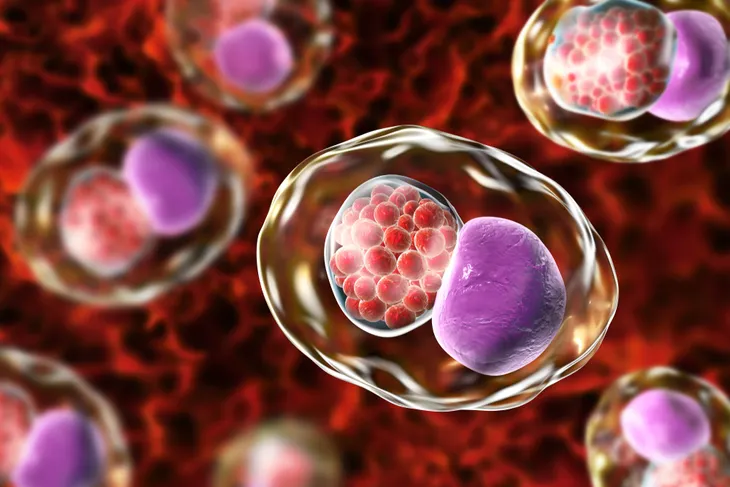
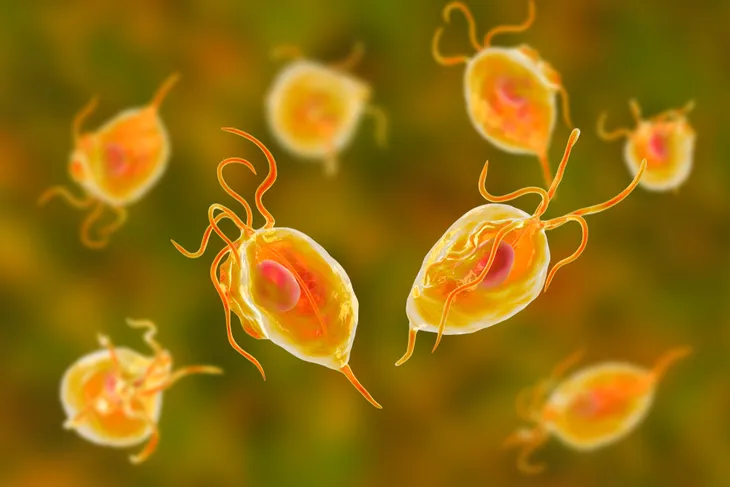
9. Trichomoniasis
Trichomoniasis is a vaginal infection caused by the parasite Trichomonas vaginalis. The majority of women with trichomoniasis complain of no symptoms. If symptoms appear, women may complain of a foul-smelling vaginal discharge, vaginal itching or irritation, and painful urination or sexual intercourse. The vaginal discharge may be gray, white, green, or yellow. The United States Centers for Disease Control and Prevention (CDC) consider trichomoniasis the most common curable STI.
Testing all pregnant women for trichomoniasis is not currently recommended. The diagnosis of infection may be confirmed by visualization of the organism in a vaginal fluid sample under a microscope. Trichomoniasis may be treated using appropriate oral antibiotics. Trichomoniasis in pregnant women has bee associated with premature (early) birth and low birth weight (infant being born weighing less than 5-pounds 8-ounces). Mother-to-child transmission of trichomoniasis is rare, but should be suspected in any female newborn observed having vaginal discharge.
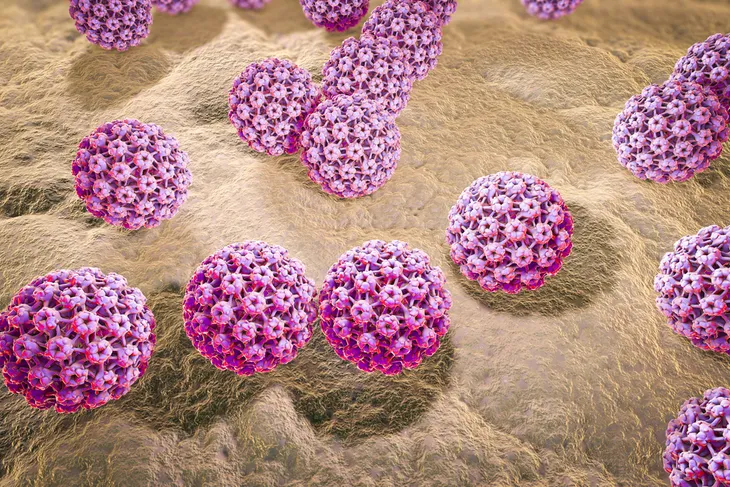
10. Genital Warts
Genital warts are a very common STI that involves the lower portion of the female reproductive tract, including the vagina, cervix, and external genitalia. They are caused by infection with the human papillomavirus (HPV). Genital warts may appear as a single bump or group of bumps in the genital area. They can be large or small, raised or flat, and some even have a cauliflower-like appearance. In some individuals, they resolve without treatment. Untreated, HPV has an association with cervical cancer.
Routing testing for genital warts is not currently recommended in pregnancy. Diagnosis of HPV may be made by visual inspection. Genital warts often increase in number and size and during pregnancy. Treatment may be delayed until after delivery. Mother-to-child transmission of genital warts is very rare. Genital warts may be prevented with vaccines.